Final ID: MP1618
Fat Mass and Systolic Blood Pressure are Modifiable CV Risk Factors Associated with Adverse Myocardial Changes in Patients with Duchenne Muscular Dystrophy
Abstract Body (Do not enter title and authors here): Introduction/Background: Patients with Duchenne muscular dystrophy (DMD) typically develop pathologic changes in body composition (increased fat mass and decreased lean mass) as well as progressive fibrofatty infiltration of the myocardium with age. These myocardial changes are clinically significant, as they contribute to the development of heart failure. In the general population, obesity and other atherosclerotic cardiovascular (CV) risk factors (RF) are linked to adverse myocardial changes (increased epicardial adipose tissue (EAT) and left ventricular mass (LVM)) as well as increased CV morbidity and mortality. However, the influence of traditional atherosclerotic CV RF on adverse myocardial changes in individuals with DMD is poorly understood.
Research Questions/Hypothesis: We aimed to determine the associations of atherosclerotic CV RF on LVM and EAT thickness on adolescents with DMD.
Methods/Approach: We conducted a single-center retrospective study of 72 males with DMD (mean age 16.1±2.5 years, 94% White) who underwent cardiac MRI and DEXA within a 3-month window between 2015–2022. Anthropometrics, DEXA, laboratory evaluation, and cardiac MRI were collected. LVM was indexed to BSA (LVMI) and EAT thickness was measured at the right atrioventricular groove at end diastole on four chamber CINE images. LVMI and TG:HDL ratio were log transformed to attain normality. Multiple linear regressions with backwards selection were performed to evaluate for which CV risk factors (fat mass index (FMI), lean mass index (LMI), systolic blood pressure (SBP), Hemoglobin A1c, LDL, and log(TG:HDL) ratio) significantly predict log(LVMI) and EAT with adjusting for race and age.
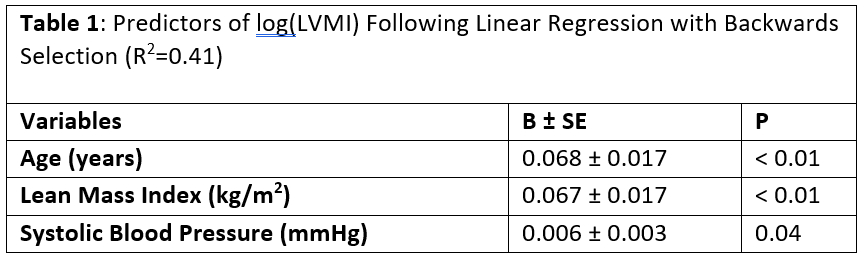
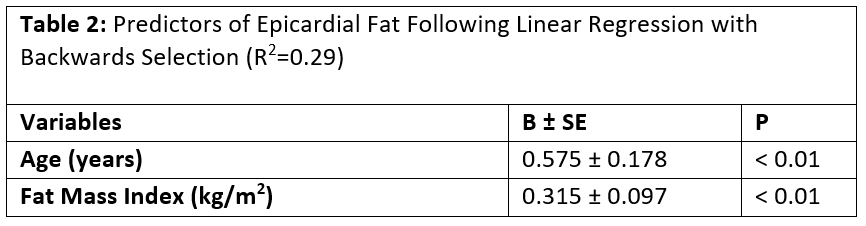
Results: LMI, SBP, and age were significantly associated with increased log(LVMI) (R2 = 0.41). FMI and age were significantly associated with greater EAT thickness (R2 = 0.29). Hemoglobin A1c, LDL, and log(TG:HDL) were not significant therefore not retained in final models.
Conclusions: SBP and body composition are associated with adverse CV changes in youth with DMD - lean mass and SBP with increased LVMI, and FMI with greater EAT. These findings underscore the importance of managing SBP and fat mass in this high-risk group. While lean mass contributes to LVMI, it remains critical to preserve motor function and quality of life. These results support incorporating CV risk assessment into routine DMD care to identify modifiable targets and help delay cardiac decline.
Research Questions/Hypothesis: We aimed to determine the associations of atherosclerotic CV RF on LVM and EAT thickness on adolescents with DMD.
Methods/Approach: We conducted a single-center retrospective study of 72 males with DMD (mean age 16.1±2.5 years, 94% White) who underwent cardiac MRI and DEXA within a 3-month window between 2015–2022. Anthropometrics, DEXA, laboratory evaluation, and cardiac MRI were collected. LVM was indexed to BSA (LVMI) and EAT thickness was measured at the right atrioventricular groove at end diastole on four chamber CINE images. LVMI and TG:HDL ratio were log transformed to attain normality. Multiple linear regressions with backwards selection were performed to evaluate for which CV risk factors (fat mass index (FMI), lean mass index (LMI), systolic blood pressure (SBP), Hemoglobin A1c, LDL, and log(TG:HDL) ratio) significantly predict log(LVMI) and EAT with adjusting for race and age.
Results: LMI, SBP, and age were significantly associated with increased log(LVMI) (R2 = 0.41). FMI and age were significantly associated with greater EAT thickness (R2 = 0.29). Hemoglobin A1c, LDL, and log(TG:HDL) were not significant therefore not retained in final models.
Conclusions: SBP and body composition are associated with adverse CV changes in youth with DMD - lean mass and SBP with increased LVMI, and FMI with greater EAT. These findings underscore the importance of managing SBP and fat mass in this high-risk group. While lean mass contributes to LVMI, it remains critical to preserve motor function and quality of life. These results support incorporating CV risk assessment into routine DMD care to identify modifiable targets and help delay cardiac decline.
More abstracts on this topic:
AI-Derived Retinal Vasculature Features Predict Cardiovascular Risk in Patients with Chronic Kidney Disease: Insights from the CRIC Study
Dhamdhere Rohan, Modanwal Gourav, Rahman Mahboob, Al-kindi Sadeer, Madabhushi Anant
Association between accelerometer-corrected physical activity and the prevalence of hypertension, diabetes, and obesity: Results from Korea National Health and Nutrition Examination Survey, 2014-2017Shin Woo Young, Choi Ji-yeob, Lee Hyo, Lee Miyoung