Final ID: Su3047
Risk factors and outcomes of postoperative atrial fibrillation in patients with congenital heart defects
Abstract Body (Do not enter title and authors here): Introduction:
Due to significant medical advances, most patients with congenital heart disease (CHD) reach adulthood, shifting CHD from a predominantly pediatric condition to a lifelong medical challenge. One of the most prevalent complications among these patients is the development of atrial fibrillation, which can occur as a postoperative complication. This study aims to investigate the incidence, risk factors and complications of postoperative atrial fibrillation after cardiac surgery in adult CHD patients.
Methods:
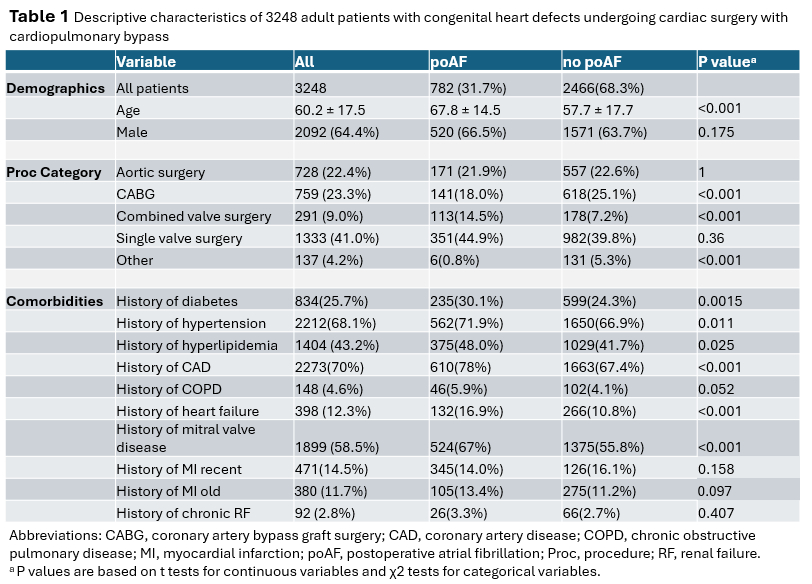
This retrospective cohort study was conducted on adult patients undergoing cardiac surgery with cardiopulmonary bypass at a tertiary care center between 2000 and 2025. 4,921 cardiac surgery patients with CHD were identified using ICD-9 and ICD-10 codes in the hospital database, and postoperative atrial fibrillation (poAF) was defined as new-onset atrial fibrillation within 30 days after surgery. 1,673 patients were excluded due to chronic AF. Logistic regression models were used to evaluate the association between risk factors such as demographic characteristics and comorbidities, and poAF, as well as the association between poAF and one-year mortality.
Results:
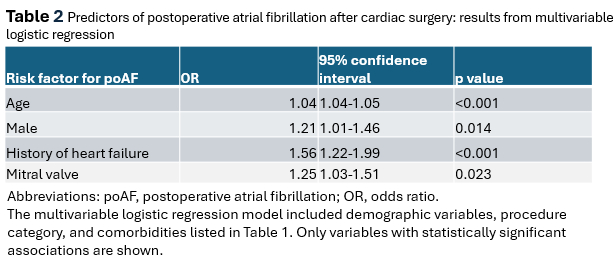
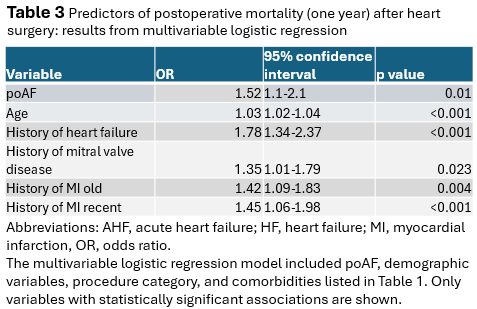
The 3,248 patients included in the study were, on average, 60.2 years old, and 64.4% were male. Most patients underwent single valve surgery, aortic surgery or coronary artery bypass grafting. Patient characteristics independently associated with an increased risk of poAF were age (OR 1.04, 95% CI 1.04-1.05), male sex (OR 1.21, 95% CI 1.01-1.46), history of heart failure (OR 1.56, 95% CI 1.22-1.99), and mitral valve disease (OR 1.25, 95% CI 1.03-1.51). Additionally, poAF was independently associated with an increased risk of one-year mortality (OR 1.52, 95% CI 1.1-2.1).
Conclusion:
In this large cohort of adults with congenital heart disease undergoing cardiac surgery, poAF was shown to be a frequent and high-impact complication, independently associated with increased postoperative mortality.
Due to significant medical advances, most patients with congenital heart disease (CHD) reach adulthood, shifting CHD from a predominantly pediatric condition to a lifelong medical challenge. One of the most prevalent complications among these patients is the development of atrial fibrillation, which can occur as a postoperative complication. This study aims to investigate the incidence, risk factors and complications of postoperative atrial fibrillation after cardiac surgery in adult CHD patients.
Methods:
This retrospective cohort study was conducted on adult patients undergoing cardiac surgery with cardiopulmonary bypass at a tertiary care center between 2000 and 2025. 4,921 cardiac surgery patients with CHD were identified using ICD-9 and ICD-10 codes in the hospital database, and postoperative atrial fibrillation (poAF) was defined as new-onset atrial fibrillation within 30 days after surgery. 1,673 patients were excluded due to chronic AF. Logistic regression models were used to evaluate the association between risk factors such as demographic characteristics and comorbidities, and poAF, as well as the association between poAF and one-year mortality.
Results:
The 3,248 patients included in the study were, on average, 60.2 years old, and 64.4% were male. Most patients underwent single valve surgery, aortic surgery or coronary artery bypass grafting. Patient characteristics independently associated with an increased risk of poAF were age (OR 1.04, 95% CI 1.04-1.05), male sex (OR 1.21, 95% CI 1.01-1.46), history of heart failure (OR 1.56, 95% CI 1.22-1.99), and mitral valve disease (OR 1.25, 95% CI 1.03-1.51). Additionally, poAF was independently associated with an increased risk of one-year mortality (OR 1.52, 95% CI 1.1-2.1).
Conclusion:
In this large cohort of adults with congenital heart disease undergoing cardiac surgery, poAF was shown to be a frequent and high-impact complication, independently associated with increased postoperative mortality.
More abstracts on this topic:
Aortic Valve Neocuspidization Using Autologous Insertion Of Pulmonary SinusTm: A Proof Of Concept
Faateh Muhammad, Raees Muhammad Aanish, Ahmed Hosam, Almiqlash Bushray, Villalobos Lizardi Jose, Ricci Marco, Ashfaq Awais
Acute Coronary Syndrome in a Patient with Situs Inversus TotalisBalani Prachi, Sharma Nitish, Ray Ayita, Sarraf Rahul, Roumia Mazen, Angelis Dimitrios