Final ID: MP355
Integrating Social Determinants of Health Into Life’s Essential 8 Framework: Enhancing Mortality Risk Prediction
Abstract Body (Do not enter title and authors here): Introduction: The Life's Essential 8 (LE8) framework proposed by the American Heart Association assesses cardiovascular health but primarily focuses on biological and behavioral factors. Social Determinants of Health (SDoHs) mainly influence health through social structures and environmental factors. Whether incorporating SDoHs into the LE8 model can improve mortality prediction remains unclear.
Methods: We established a retrospective cohort using data from the 2005–2018 National Health and Nutrition Examination Survey (NHANES). Weighted Cox proportional hazards models were employed to assess associations between SDoHs and mortality, adjusting for confounders and LE8 scores. Interaction effects were quantified using the relative excess risk due to interaction (RERI). Predictive performance improvements were evaluated via continuous net reclassification improvement (NRI) and integrated discrimination improvement (IDI) indices for all-cause and cardiovascular mortality.
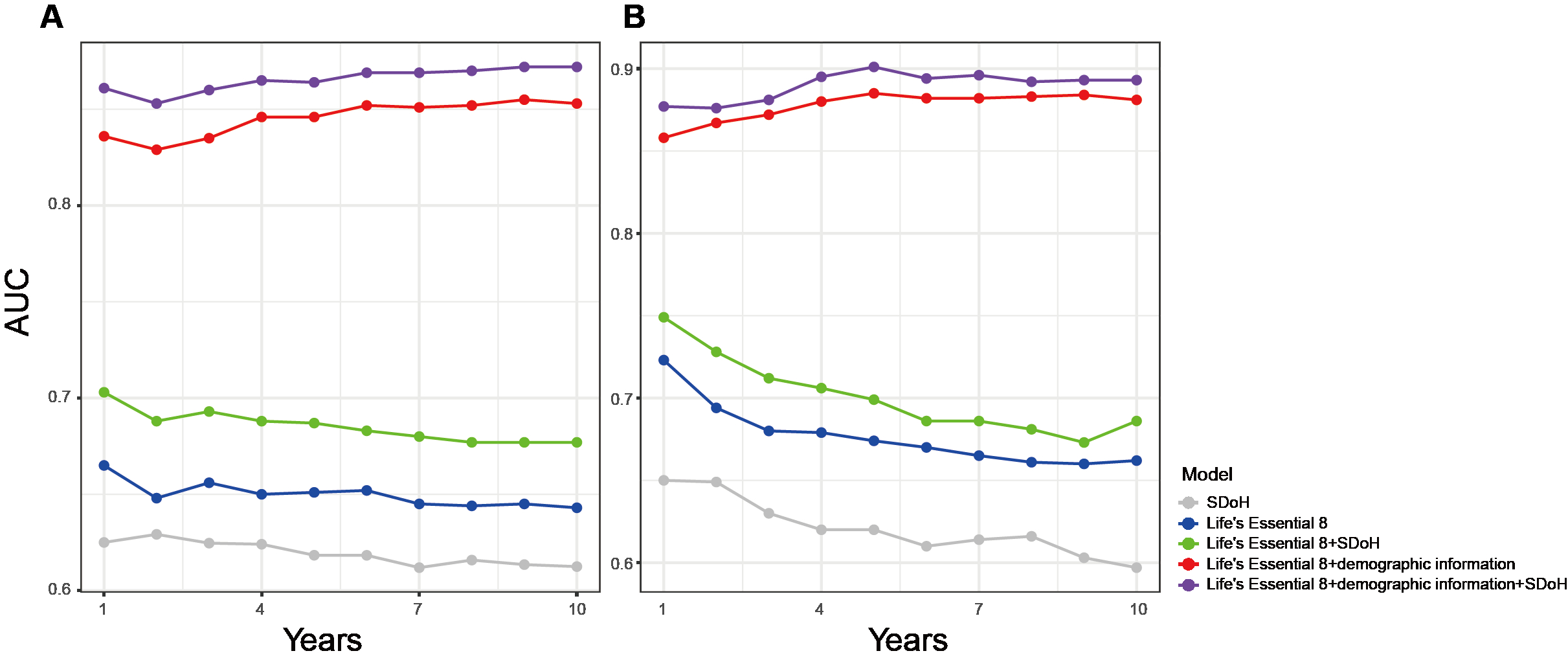
Results: Among 22,938 participants (representing 142 million U.S. adults; mean age 47.6 years; 51.6% female), 2,344 all-cause deaths (7.29%) and 720 cardiovascular deaths (2.12%) occurred over a median follow-up of 7.83 years. Multivariable analysis identified unemployment (HR = 1.44, 95% CI: 1.25–1.66, P < 0.001), low-income status (poverty-to-income ratio <1.3; HR = 1.75, 95% CI: 1.32–2.31, P < 0.001), severe food insecurity (HR = 1.45, 95% CI: 1.19–1.78, P < 0.001), and being unmarried/living alone (HR = 1.43, 95% CI: 1.28–1.59, P < 0.001) as significant predictors of all-cause mortality. Low-income status (HR = 1.90, 95% CI: 1.21–2.97, P = 0.010) and being unmarried/living alone (HR = 1.52, 95% CI: 1.26–1.85, P < 0.001) also independently predicted cardiovascular mortality. Synergistic interactions were observed between unemployment and low-income status (RERI = 0.90), food insecurity (RERI = 0.59), and unmarried/living alone status (RERI = 0.37) for all-cause mortality. Low-income status combined with unmarried/living alone status exhibited additive effects on cardiovascular mortality (RERI = 0.46). Integrating SDoHs significantly improved 1-, 3-, 5-, and 10-year mortality prediction for both outcomes (NRI and IDI P < 0.05).
Conclusion: Incorporating selected SDoHs into the LE8 framework enhances the predictive ability for both all-cause and cardiovascular mortality risks.
Methods: We established a retrospective cohort using data from the 2005–2018 National Health and Nutrition Examination Survey (NHANES). Weighted Cox proportional hazards models were employed to assess associations between SDoHs and mortality, adjusting for confounders and LE8 scores. Interaction effects were quantified using the relative excess risk due to interaction (RERI). Predictive performance improvements were evaluated via continuous net reclassification improvement (NRI) and integrated discrimination improvement (IDI) indices for all-cause and cardiovascular mortality.
Results: Among 22,938 participants (representing 142 million U.S. adults; mean age 47.6 years; 51.6% female), 2,344 all-cause deaths (7.29%) and 720 cardiovascular deaths (2.12%) occurred over a median follow-up of 7.83 years. Multivariable analysis identified unemployment (HR = 1.44, 95% CI: 1.25–1.66, P < 0.001), low-income status (poverty-to-income ratio <1.3; HR = 1.75, 95% CI: 1.32–2.31, P < 0.001), severe food insecurity (HR = 1.45, 95% CI: 1.19–1.78, P < 0.001), and being unmarried/living alone (HR = 1.43, 95% CI: 1.28–1.59, P < 0.001) as significant predictors of all-cause mortality. Low-income status (HR = 1.90, 95% CI: 1.21–2.97, P = 0.010) and being unmarried/living alone (HR = 1.52, 95% CI: 1.26–1.85, P < 0.001) also independently predicted cardiovascular mortality. Synergistic interactions were observed between unemployment and low-income status (RERI = 0.90), food insecurity (RERI = 0.59), and unmarried/living alone status (RERI = 0.37) for all-cause mortality. Low-income status combined with unmarried/living alone status exhibited additive effects on cardiovascular mortality (RERI = 0.46). Integrating SDoHs significantly improved 1-, 3-, 5-, and 10-year mortality prediction for both outcomes (NRI and IDI P < 0.05).
Conclusion: Incorporating selected SDoHs into the LE8 framework enhances the predictive ability for both all-cause and cardiovascular mortality risks.
More abstracts on this topic:
A machine learning approach to examining the associations of minority stressors and physical activity among sexual and gender minority adults
Lopez Veneros David, Ensari Ipek, Bhilegaonkar Riya, Sharma Yashika, Caceres Billy
Achieving Guidelines within a 24-Hour Movement Paradigm and Risk of Cardiovascular Disease and All-Cause Mortality in United States AdultsBoudreaux Benjamin, Xu Chang, Dooley Erin, Hornikel Bjoern, Munson Alexandra, Shechter Ari, Palta Priya, Gabriel Kelley, Diaz Keith