Final ID: MP763
Heart Transplant Outcomes in Donor After Circulatory Death vs Donor After Brain Death Donors for Patients Bridged with HeartMate 3 Devices.
Abstract Body (Do not enter title and authors here): Introduction: The number of heart transplants (HT) with donor after circulatory death (DCD) donors has increased. Outcomes for DCD donors compared to donor after brain death (DBD) donors have not been fully explored in patients bridged with HeartMate 3 (HM3) left ventricular assist devices (Abbott, Chicago, IL). This study aims to assess short and long-term survival outcomes in DCD vs DBD HT in patients bridged with HM3.
Methods: All adults ≥ 18 years bridged to HT with HM3 between October 18, 2018 and March 31, 2025 were identified from the UNOS database. Patients were stratified by donor type (DCD vs DBD). Primary outcome was 90-day, 1-year and 3-year survival. Multivariable analysis was performed for risk-adjustment.
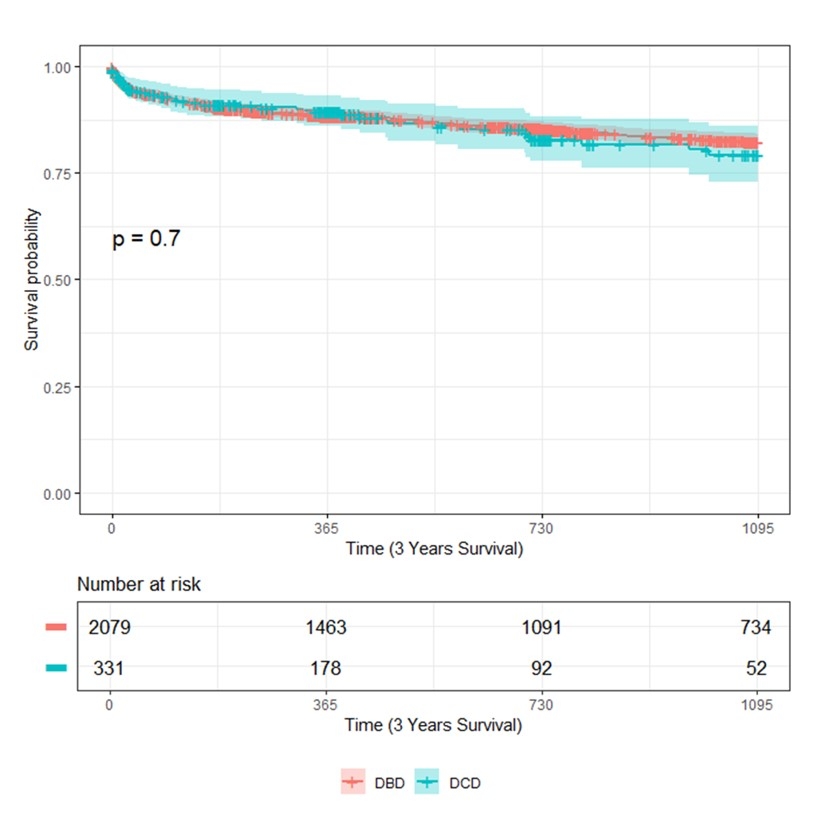
Results: Following exclusion, 2416 patients (332 DCD and 2084 DBD) were identified for analysis. DCD patients had longer duration of HM3 support [658.5 (336.5, 1122) vs 535 (294.5, 912.5), p 0.001], more frequently male (82.2% vs 77.4%, p 0.046), had fewer days on waitlist [81.5 (19.5, 334) vs 137.5 (32, 426), p 0.002], more frequently blood type O (54.2% vs 38.4%, p <0.001), and more frequently status 4 listing (44.0% vs 35.2%, p<0.0001). DCD donors were younger [33 (25.5, 39) vs 35 (27, 43), p 0.011], more frequently male (83.4% vs 70.7%, p < 0.0001) and more likely to die of trauma (38.0% vs 31.7%, p 0.035). There was no difference in survival between DCD and DBD patients at 90 days (93.4 % vs 93.0%, p 0.8272), 1 year (90.6% vs 89.0%, p 0.3823) or 3 years (87.0% vs 85.3%, p 0.4194). Further, there was no difference in secondary outcomes in DCD vs DBD patients including post-HT LOS [17 days (13, 26) vs 18 days (13, 28), p 0.5262], acute rejection (10.6% vs 8.7%, p 0.2617), acute renal failure (18.1% vs 16.3%, p 0.4141), stroke (3.3% vs 4.8%, p 0.2284), or pacemaker implant (1.2% vs 1.9%, p 0.3933). Predictors of 1-year mortality included longer time on HM3 support [HR 1.02 (1.0-1.04), p 0.013], increased age of recipient [HR 1.03 (1.02-1.5), p <0.001], female recipient [HR 1.59 (1.2-2.12), p 0.001], recipient diabetes [HR 1.33 (1.04-1.71), p 0.025], pre-operative inotrope support [HR 1.49 (1.0-2.21), p 0.048], elevated creatinine [HR 1.21 (1.03-1.41), p 0.017], and ICU status [HR 1.43 (1.01-2.02), p 0.042].
Conclusion: Morbidity and mortality is similar between DCD and DBD HT in patients bridged with HM3. Multivariable analysis reveals certain factors impacting mortality such as duration of HM3 support that warrant further exploration.
Methods: All adults ≥ 18 years bridged to HT with HM3 between October 18, 2018 and March 31, 2025 were identified from the UNOS database. Patients were stratified by donor type (DCD vs DBD). Primary outcome was 90-day, 1-year and 3-year survival. Multivariable analysis was performed for risk-adjustment.
Results: Following exclusion, 2416 patients (332 DCD and 2084 DBD) were identified for analysis. DCD patients had longer duration of HM3 support [658.5 (336.5, 1122) vs 535 (294.5, 912.5), p 0.001], more frequently male (82.2% vs 77.4%, p 0.046), had fewer days on waitlist [81.5 (19.5, 334) vs 137.5 (32, 426), p 0.002], more frequently blood type O (54.2% vs 38.4%, p <0.001), and more frequently status 4 listing (44.0% vs 35.2%, p<0.0001). DCD donors were younger [33 (25.5, 39) vs 35 (27, 43), p 0.011], more frequently male (83.4% vs 70.7%, p < 0.0001) and more likely to die of trauma (38.0% vs 31.7%, p 0.035). There was no difference in survival between DCD and DBD patients at 90 days (93.4 % vs 93.0%, p 0.8272), 1 year (90.6% vs 89.0%, p 0.3823) or 3 years (87.0% vs 85.3%, p 0.4194). Further, there was no difference in secondary outcomes in DCD vs DBD patients including post-HT LOS [17 days (13, 26) vs 18 days (13, 28), p 0.5262], acute rejection (10.6% vs 8.7%, p 0.2617), acute renal failure (18.1% vs 16.3%, p 0.4141), stroke (3.3% vs 4.8%, p 0.2284), or pacemaker implant (1.2% vs 1.9%, p 0.3933). Predictors of 1-year mortality included longer time on HM3 support [HR 1.02 (1.0-1.04), p 0.013], increased age of recipient [HR 1.03 (1.02-1.5), p <0.001], female recipient [HR 1.59 (1.2-2.12), p 0.001], recipient diabetes [HR 1.33 (1.04-1.71), p 0.025], pre-operative inotrope support [HR 1.49 (1.0-2.21), p 0.048], elevated creatinine [HR 1.21 (1.03-1.41), p 0.017], and ICU status [HR 1.43 (1.01-2.02), p 0.042].
Conclusion: Morbidity and mortality is similar between DCD and DBD HT in patients bridged with HM3. Multivariable analysis reveals certain factors impacting mortality such as duration of HM3 support that warrant further exploration.
More abstracts on this topic:
A Case of Dilated Cardiomyopathy and Systemic Thromboembolism in a Young Patient on Testosterone Replacement Therapy
Sabri Muhammad, Ijaz Naila, Nadeem Ramsha, Checchio Lucy, Riaz Faiza
β1-adrenergic autoantibodies (β1-AA) augment macropinocytosis in CD4+ T cells, leading to the expansion of CD4+CD28− T cell subsets in heart failure.Sun Fei, Yao Junyan, Li Bingjie, Zhang Suli, Liu Huirong