Final ID: MP1326
A National Analysis Of Heart Donation After Circulatory Death In The United States
Abstract Body (Do not enter title and authors here): Background:
Heart transplantation (HTx) is the gold-standard therapy for refractory heart failure; however, this life-saving procedure remains greatly limited in the setting of an ongoing donor shortage coupled with an aging patient population’s increasing demand for transplantation. In an effort to address this supply-demand mismatch, many transplant centers have eased previous contraindications to donation; for instance, by accepting donors with active infectious disease or older age. An area of active research in the field of HTx is utilizing donation after circulatory death (DCD). While there has been extensive evidence from international studies to suggest DCD hearts have similar outcomes compared to donation after brain death (DBD), there is scarce data on DCD procurement outcomes in the United States after its incorporation into allocation policy in 2019, particularly using a follow-up period greater than 1-year.
Research question:
Do recipients with DCD and DBD heart procurements have similar survival outcome in the U.S.?
Goals:
Our goal is to compare and assess heart DCD outcomes in an effort to help mitigate the ongoing donor shortage in the United States.
Methods:
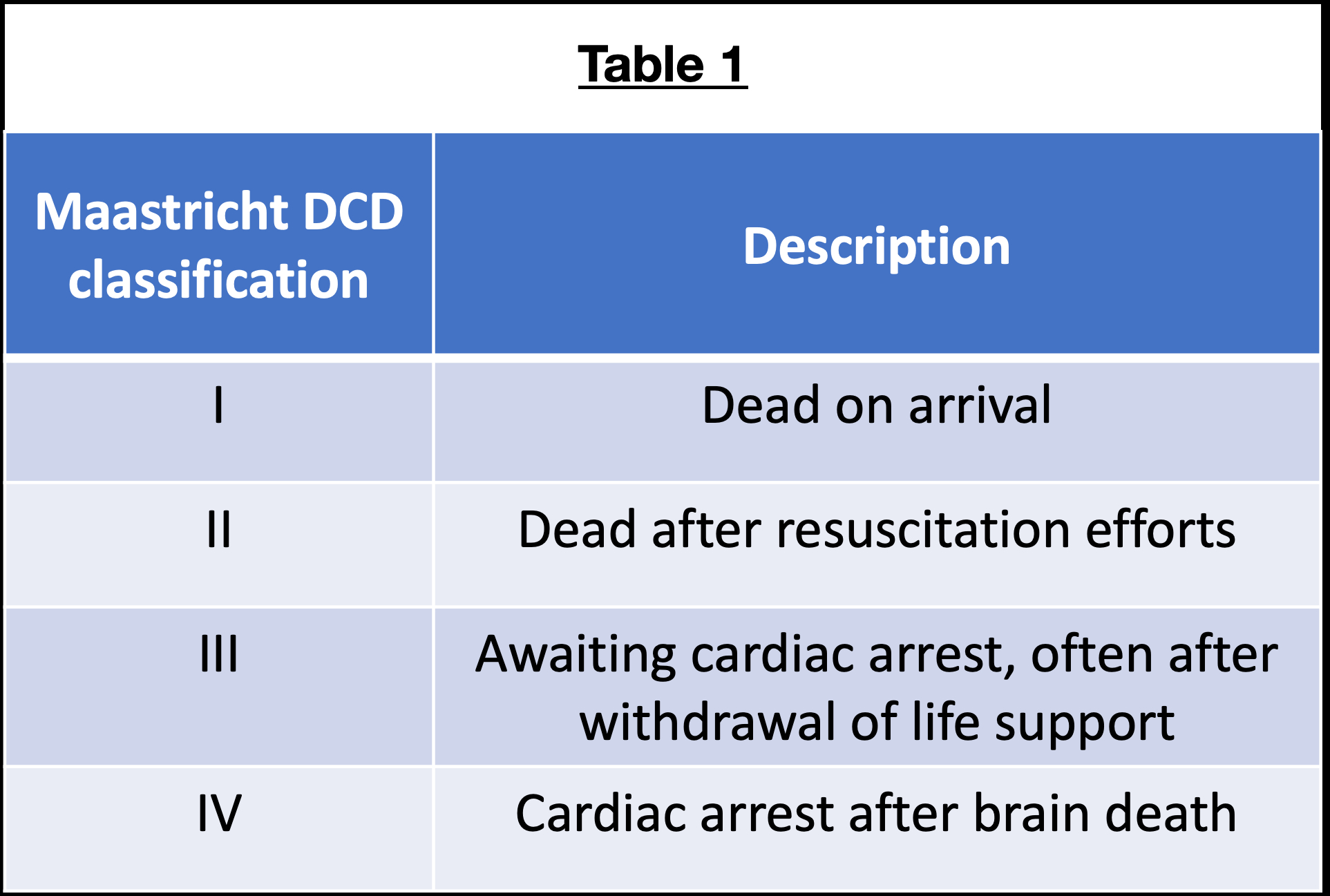
The UNOS database was queried for adult orthotopic HTx recipients who were transplanted between 1/1/2019 to 8/31/2023. Heart retransplants, multiorgan transplants, or patients with VAD/TAH or on ECMO were excluded. Patients were categorized into three groups based on Maastricht classification, which is further described in Table 1: DBD, DCD III, and DCD IV. Survival outcome during a 2-year follow-up period was assessed utilizing Kaplan-Meier survival curves, log-rank test, and Cox regression model.
Results:
A total of 9,444 recipients were included in our investigation, of which 86.8% was DBD, 6.5% DCD III, and 6.8% DCD IV. Kaplan-Meier survival curves are displayed in Figure 1. Survival estimates at 2-years for each group are: DBD: 87.8%; DCD III: 84.9%; DCD IV: 88.8%. Log-rank test found no significant difference in survival between groups (p=0.485). This finding was supported by Cox regression model, which found no significant difference in mortality risk with reference to DBD for both DCD III (HR=1.13, p=0.429) and DCD IV (HR=0.89, p=0.393) groups.
Conclusion:
Our investigation found that both DCD III and IV have similar survival outcome as DBD groups in the U.S. population. These results further support the use of DCD heart procurement in an effort to increase the available donor pool.
Heart transplantation (HTx) is the gold-standard therapy for refractory heart failure; however, this life-saving procedure remains greatly limited in the setting of an ongoing donor shortage coupled with an aging patient population’s increasing demand for transplantation. In an effort to address this supply-demand mismatch, many transplant centers have eased previous contraindications to donation; for instance, by accepting donors with active infectious disease or older age. An area of active research in the field of HTx is utilizing donation after circulatory death (DCD). While there has been extensive evidence from international studies to suggest DCD hearts have similar outcomes compared to donation after brain death (DBD), there is scarce data on DCD procurement outcomes in the United States after its incorporation into allocation policy in 2019, particularly using a follow-up period greater than 1-year.
Research question:
Do recipients with DCD and DBD heart procurements have similar survival outcome in the U.S.?
Goals:
Our goal is to compare and assess heart DCD outcomes in an effort to help mitigate the ongoing donor shortage in the United States.
Methods:
The UNOS database was queried for adult orthotopic HTx recipients who were transplanted between 1/1/2019 to 8/31/2023. Heart retransplants, multiorgan transplants, or patients with VAD/TAH or on ECMO were excluded. Patients were categorized into three groups based on Maastricht classification, which is further described in Table 1: DBD, DCD III, and DCD IV. Survival outcome during a 2-year follow-up period was assessed utilizing Kaplan-Meier survival curves, log-rank test, and Cox regression model.
Results:
A total of 9,444 recipients were included in our investigation, of which 86.8% was DBD, 6.5% DCD III, and 6.8% DCD IV. Kaplan-Meier survival curves are displayed in Figure 1. Survival estimates at 2-years for each group are: DBD: 87.8%; DCD III: 84.9%; DCD IV: 88.8%. Log-rank test found no significant difference in survival between groups (p=0.485). This finding was supported by Cox regression model, which found no significant difference in mortality risk with reference to DBD for both DCD III (HR=1.13, p=0.429) and DCD IV (HR=0.89, p=0.393) groups.
Conclusion:
Our investigation found that both DCD III and IV have similar survival outcome as DBD groups in the U.S. population. These results further support the use of DCD heart procurement in an effort to increase the available donor pool.
More abstracts on this topic:
A Case of Steroid-Refractory Immune-checkpoint-inhibitor Induced Myocarditis Responsive to Mycophenolate and Anti-thymocyte globulin
Dabdoub Jorge, Wilson Michael, Gottbrecht Matthew, Salazar Ryan, Shih Jeffrey
Foxe1 Loss of Function Contributes to Adverse Remodeling in the HeartWidiapradja Alexander, Connery Heather, Bullock Martyn, Clifton-bligh Roderick, Levick Scott