Final ID: MP1023
Left Atrial Appendage Occlusion Is Safe and Effective in Cardiac Amyloidosis: Real-World Single-Center Experience
Abstract Body (Do not enter title and authors here): Background:
Cardiac amyloidosis (CA) is associated with increased thromboembolic risk, particularly in patients with atrial fibrillation (AF), who often also have high bleeding risk. Left atrial appendage closure (LAAC) offers an alternative to oral anticoagulation (OAC) in high-bleeding-risk AF patients, but data about its safety and efficacy in CA patients remain limited. This study evaluates procedural success, safety, and clinical outcomes of LAAC in CA patients
Methods:
We conducted a retrospective chart review study of patients with confirmed CA who underwent LAAC at the Cleveland Clinic Foundation (CCF) between January 2014 and December 2024. Procedural success, peri-device leak (PDL), thromboembolic, and bleeding events were assessed. Peri-device leak (PDL) was defined as flow around the implanted device into the left atrial appendage. Event-free survival (EFS) was defined from the time of implantation to the occurrence of a major bleeding event, Stroke/TIA, or death.
Results:
A total of 21 patients were identified, with 90.5% being of the wild-type transthyretin amyloidosis type. The mean age at the time of procedure was 82 ± 6 years, and 100% of the cohort was white. The mean CHA2DS2-VASc score was 4 ± 1, and the mean HAS-BLED score was 3.5 ± 1.3. Five patients (~24%) had a history of at least one ischemic stroke or TIA.
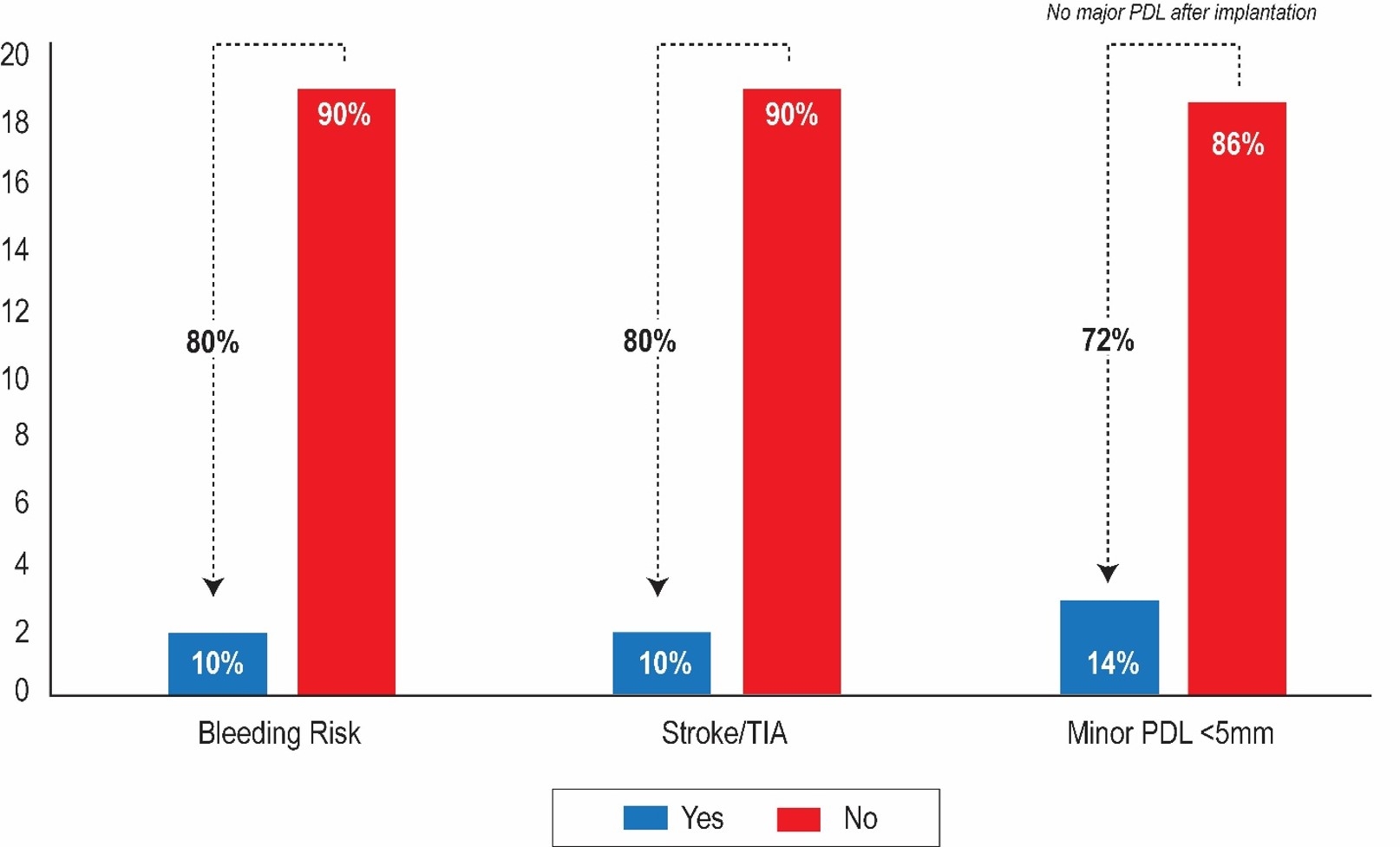
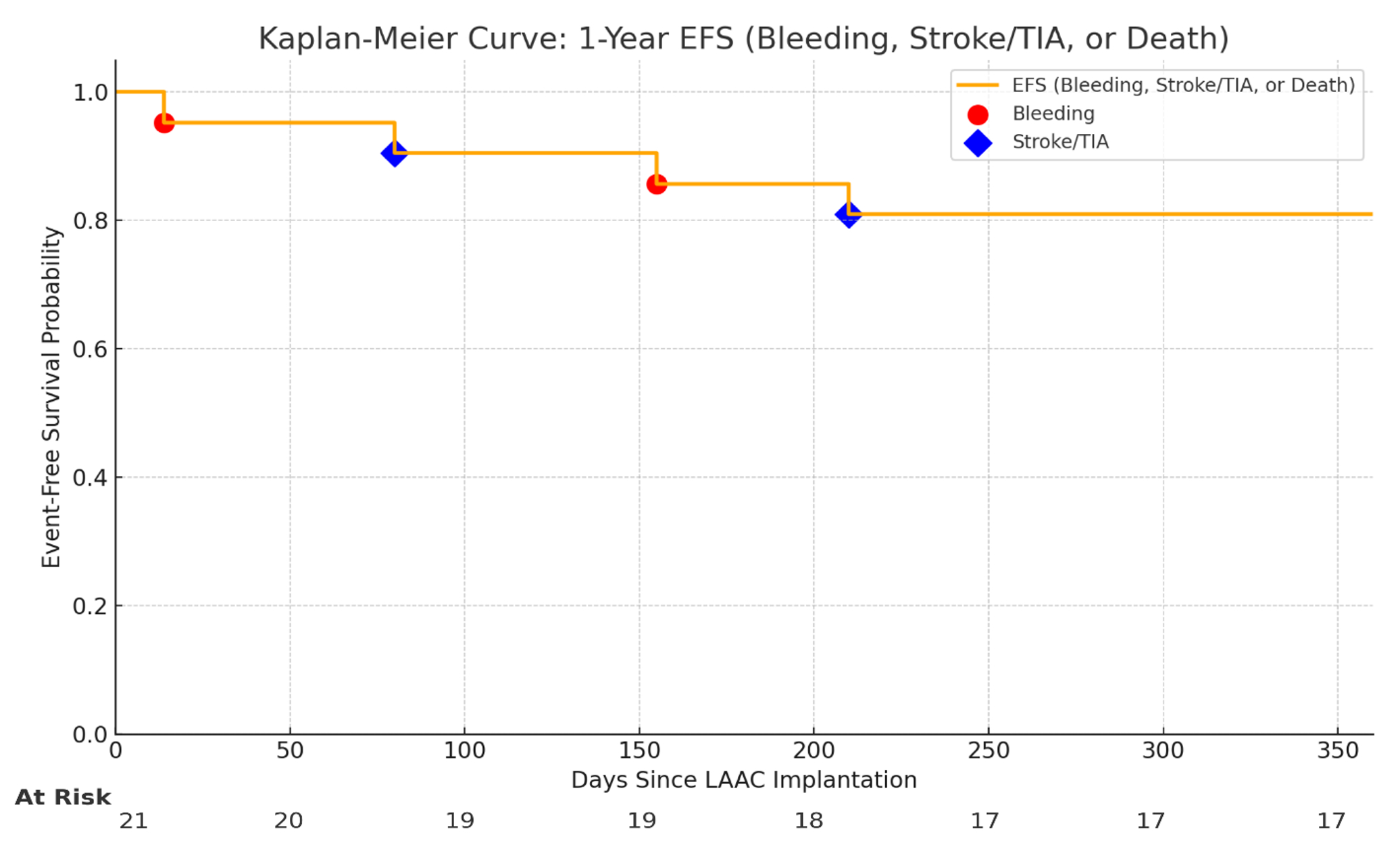
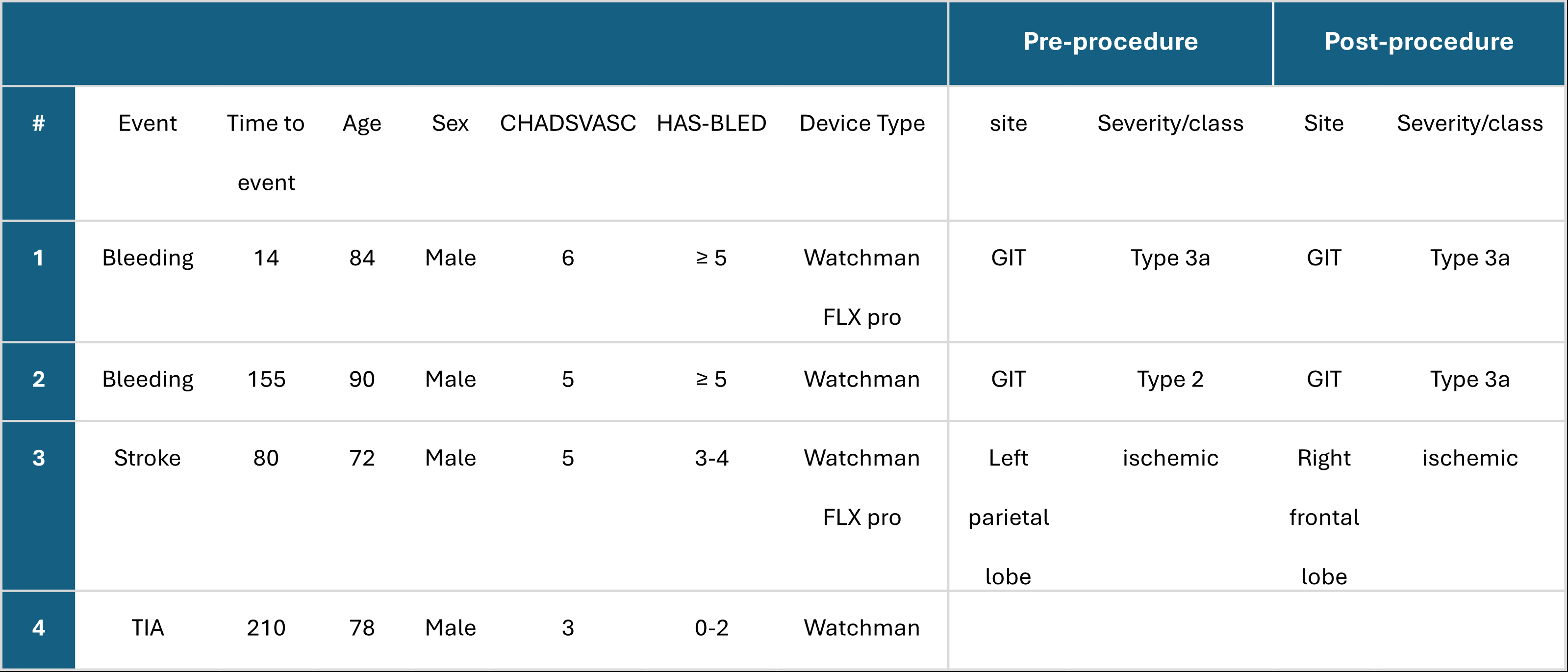
Procedural success was achieved in 95% of patients, with only one case aborted due to the persistence of an LAA thrombus despite anticoagulation therapy. No intra- or peri-procedural complications were observed. An immediate complete seal was achieved in all patients, with no PDL noted. At a median follow-up of 24 months (IQR: 14-30), minor PDL (≤5 mm) developed in 3 patients (14.3%), with no major leaks (>5 mm) observed and no device-related thrombosis (DRT) (Figure 1). Two patients (9.5%) experienced post-procedural major bleeding; both were on OAC at the time of bleeding and had a prior history of bleeding at the same site. Two patients (9.5%) experienced ischemic stroke or TIA, both with prior ischemic stroke/TIA history (Table 1). The 12-month and 2-year EFS were both 81% (Figure 2).
Conclusion:
In CA patients, LAAC demonstrated high procedural success and low complication rates, suggesting it is a safe and feasible approach for stroke prevention. However, vigilance for potential complications, such as peri-device leaks, is needed. Larger, multicenter studies are needed to validate these findings and further assess long-term safety
Cardiac amyloidosis (CA) is associated with increased thromboembolic risk, particularly in patients with atrial fibrillation (AF), who often also have high bleeding risk. Left atrial appendage closure (LAAC) offers an alternative to oral anticoagulation (OAC) in high-bleeding-risk AF patients, but data about its safety and efficacy in CA patients remain limited. This study evaluates procedural success, safety, and clinical outcomes of LAAC in CA patients
Methods:
We conducted a retrospective chart review study of patients with confirmed CA who underwent LAAC at the Cleveland Clinic Foundation (CCF) between January 2014 and December 2024. Procedural success, peri-device leak (PDL), thromboembolic, and bleeding events were assessed. Peri-device leak (PDL) was defined as flow around the implanted device into the left atrial appendage. Event-free survival (EFS) was defined from the time of implantation to the occurrence of a major bleeding event, Stroke/TIA, or death.
Results:
A total of 21 patients were identified, with 90.5% being of the wild-type transthyretin amyloidosis type. The mean age at the time of procedure was 82 ± 6 years, and 100% of the cohort was white. The mean CHA2DS2-VASc score was 4 ± 1, and the mean HAS-BLED score was 3.5 ± 1.3. Five patients (~24%) had a history of at least one ischemic stroke or TIA.
Procedural success was achieved in 95% of patients, with only one case aborted due to the persistence of an LAA thrombus despite anticoagulation therapy. No intra- or peri-procedural complications were observed. An immediate complete seal was achieved in all patients, with no PDL noted. At a median follow-up of 24 months (IQR: 14-30), minor PDL (≤5 mm) developed in 3 patients (14.3%), with no major leaks (>5 mm) observed and no device-related thrombosis (DRT) (Figure 1). Two patients (9.5%) experienced post-procedural major bleeding; both were on OAC at the time of bleeding and had a prior history of bleeding at the same site. Two patients (9.5%) experienced ischemic stroke or TIA, both with prior ischemic stroke/TIA history (Table 1). The 12-month and 2-year EFS were both 81% (Figure 2).
Conclusion:
In CA patients, LAAC demonstrated high procedural success and low complication rates, suggesting it is a safe and feasible approach for stroke prevention. However, vigilance for potential complications, such as peri-device leaks, is needed. Larger, multicenter studies are needed to validate these findings and further assess long-term safety
More abstracts on this topic:
30-Day Outcomes of Dual vs Triple Antithrombotic Therapy After PCI
Meeks William, Slone Sarah, Barringhaus Kurt
A Small, Convenient, and Calibration-Free Absolute Blood Pressure Measurement Device Based on the Oscillometric MethodInan Omer, Ozmen Goktug, Berkebile John, Dubuque Shaun, Tourian Dikran, Chan Michael