Final ID: MP1206
Oxygen Levels During Cardiopulmonary Bypass - Comparing Hyperoxia and Normoxia in Adult Cardiac Surgery: A Systematic Review and Meta-analysis
Abstract Body (Do not enter title and authors here): Background:
The remarkable innovations in cardiac surgery enable surgeons to operate on a still heart while maintaining perfusion to vital organs. To offset reduced cardiac output during Cardiopulmonary Bypass (CPB), high-flow oxygen is often used to increase arterial oxygen content. However, supraphysiologic oxygen levels may promote oxidative stress, potentially exacerbating inflammation and ischemia-reperfusion injury. We conducted a meta-analysis to compare the impact of hyperoxia versus normoxia during CPB on clinical outcomes in adult cardiac surgery.
Methods:
We systematically searched PubMed, SCOPUS, and Google Scholar from inception to November 12, 2024, following PRISMA guidelines and PROSPERO registration [CRD42024XXXX]. Eligible studies included randomised controlled trials (RCTs) or cohort studies comparing hyperoxia versus normoxia during CPB in adults undergoing cardiac surgery. Primary outcomes included mean operative time, postoperative arrhythmias, cardiac arrest, vasoactive medication use, cardiac troponin, length of stay (hospital and ICU), mortality, and major complications. Meta-analysis was conducted using Review Manager (v5.4.1) with mean difference or risk ratio estimates and 95% confidence intervals. Sensitivity analyses and publication bias assessments were performed.
Results:
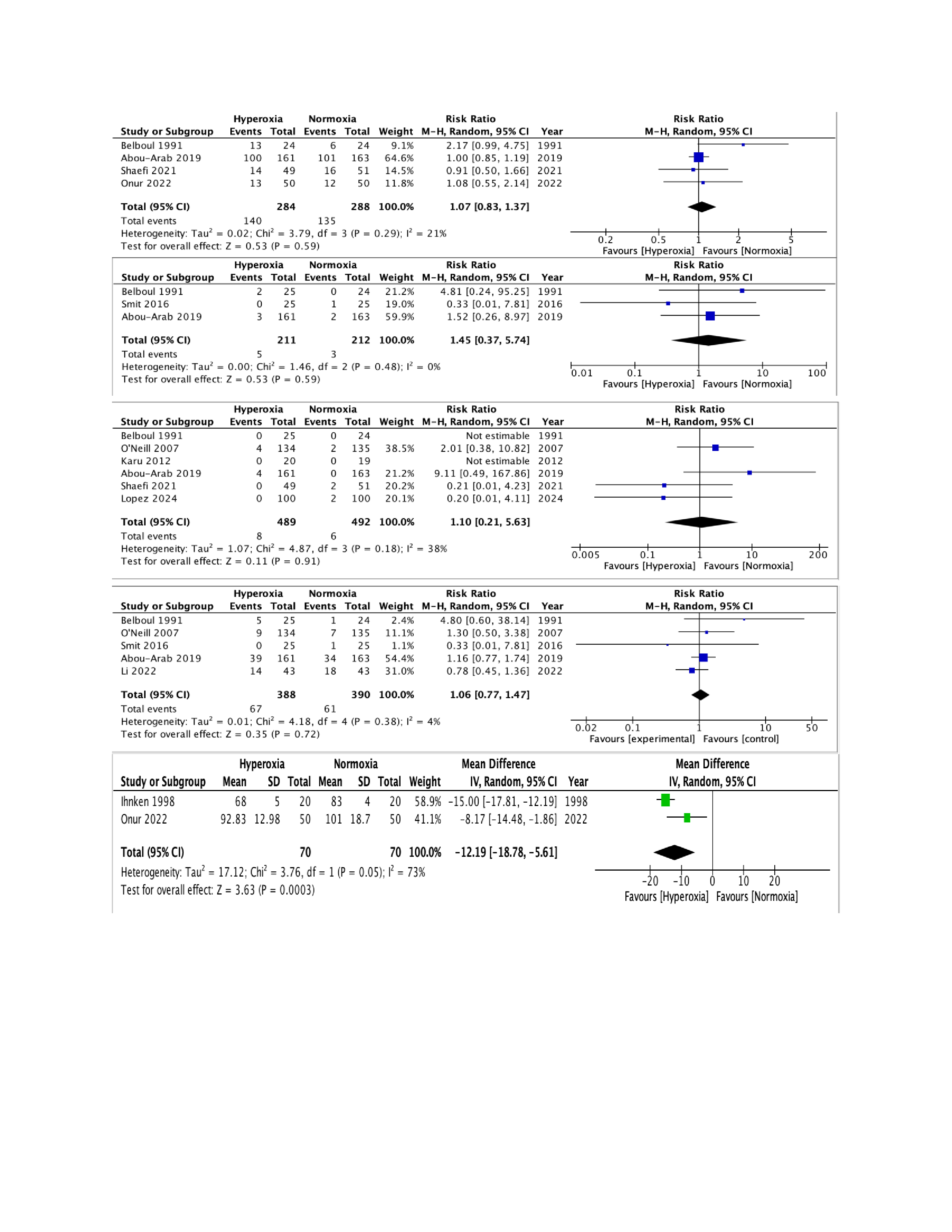
Eighteen studies (17 RCTs and 1 prospective study) with a total of 1,767 patients (882 hyperoxia; 885 ica) were included. Across all outcomes analyzed—including postoperative arrhythmias (RR 1.07, 95% CI 0.83–1.37), cardiac arrest (RR 1.45, 95% CI 0.37–5.74), in-hospital mortality (RR 1.10, 95% CI 0.21–5.63), and complications (RR 1.06, 95% CI 0.77–1.47)—no significant differences were observed. Sensitivity analyses for hospital and ICU stay durations confirmed the robustness of these findings. Notably, hyperoxia was associated with a statistically significant increase in postoperative forced vital capacity (FVC) (RR -12.19, 95% CI -18.78 to -5.06).
Conclusion:
While hyperoxia was associated with a significant increase in postoperative FVC, it did not meaningfully affect complications, mortality, or recovery time as compared to normoxia. Therefore, the overall evidence does not support a strong clinical advantage for either strategy. These findings highlight the need for further long-term studies with a standardized definition of hyperoxia and continuous PaO2 monitoring to establish an optimal intraoperative oxygenation strategy.
The remarkable innovations in cardiac surgery enable surgeons to operate on a still heart while maintaining perfusion to vital organs. To offset reduced cardiac output during Cardiopulmonary Bypass (CPB), high-flow oxygen is often used to increase arterial oxygen content. However, supraphysiologic oxygen levels may promote oxidative stress, potentially exacerbating inflammation and ischemia-reperfusion injury. We conducted a meta-analysis to compare the impact of hyperoxia versus normoxia during CPB on clinical outcomes in adult cardiac surgery.
Methods:
We systematically searched PubMed, SCOPUS, and Google Scholar from inception to November 12, 2024, following PRISMA guidelines and PROSPERO registration [CRD42024XXXX]. Eligible studies included randomised controlled trials (RCTs) or cohort studies comparing hyperoxia versus normoxia during CPB in adults undergoing cardiac surgery. Primary outcomes included mean operative time, postoperative arrhythmias, cardiac arrest, vasoactive medication use, cardiac troponin, length of stay (hospital and ICU), mortality, and major complications. Meta-analysis was conducted using Review Manager (v5.4.1) with mean difference or risk ratio estimates and 95% confidence intervals. Sensitivity analyses and publication bias assessments were performed.
Results:
Eighteen studies (17 RCTs and 1 prospective study) with a total of 1,767 patients (882 hyperoxia; 885 ica) were included. Across all outcomes analyzed—including postoperative arrhythmias (RR 1.07, 95% CI 0.83–1.37), cardiac arrest (RR 1.45, 95% CI 0.37–5.74), in-hospital mortality (RR 1.10, 95% CI 0.21–5.63), and complications (RR 1.06, 95% CI 0.77–1.47)—no significant differences were observed. Sensitivity analyses for hospital and ICU stay durations confirmed the robustness of these findings. Notably, hyperoxia was associated with a statistically significant increase in postoperative forced vital capacity (FVC) (RR -12.19, 95% CI -18.78 to -5.06).
Conclusion:
While hyperoxia was associated with a significant increase in postoperative FVC, it did not meaningfully affect complications, mortality, or recovery time as compared to normoxia. Therefore, the overall evidence does not support a strong clinical advantage for either strategy. These findings highlight the need for further long-term studies with a standardized definition of hyperoxia and continuous PaO2 monitoring to establish an optimal intraoperative oxygenation strategy.
More abstracts on this topic:
A Systematic Review and Meta-Analysis on the Anesthetic Approaches for Left Atrial Appendage Occlusion: Comparing Conscious Sedation and General Anesthesia
Zaidi Syed Rafay, Ajmal Umna, Rauf Zainab, Maaz Muhammad, Gulzar Sara, Burki Shahid, Nazir Abubakar, Mirza Azka, Hassan Ahmad, Amir Maaz, Jahangir Muhammad Asad, Rasul Minahil, Raza Muhammad, Malik Mohammad
A rare case of ventriculobronchial fistula caused by an epicardial defibrillator patchAlampoondi Venkataramanan Sai Vikram, Windle John