Final ID: Sa1011
Hemodynamics and Extracardiac Causes of Cardiac Tamponade: A Diagnostic and Therapeutic Dilemma Authors: Shan Zaidi, BS1; Nikita Jhawar, MD2; Vivek Kulkarni, MD, MHS, EdM, FACC1,3 Author Affiliations: 1Cooper Medical School of Rowan University, Camden, New Jersey 08103 2,3Department of Cardiovascular Disease, Cooper University Hospital, Camden, New Jersey 08103
Abstract Body (Do not enter title and authors here): Background:
Cardiac tamponade is a known hemodynamic complication of pericardial effusion. However, other less recognized etiologies can produce similar physiologic findings and require a distinct diagnostic and therapeutic approach. Accurate identification of the underlying cause of tamponade is essential for effective management.
Case Summary:
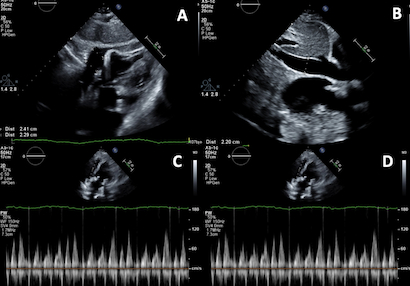
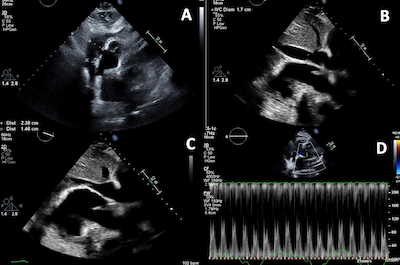
A 68-year-old woman, one month after bioprosthetic mitral valve replacement for severe mitral regurgitation, presented with fatigue and mild dyspnea on exertion. She was hypotensive and tachycardic, with pulsus paradoxus on exam. Transthoracic echocardiogram revealed a small anterior pericardial effusion and echocardiographic features consistent with tamponade physiology. A large right-sided pleural effusion was also discovered on CT imaging. She underwent urgent thoracentesis, after which tamponade findings resolved, and her symptoms markedly improved without pericardiocentesis.
Discussion:
This case highlights an uncommon but clinically significant cause of tamponade physiology: extracardiac compression from a large pleural effusion. While tamponade is usually due to pericardial fluid, elevated intrathoracic pressure from a pleural effusion can similarly impair diastolic filling and cause classic tamponade. The presence of a small pericardial effusion initially raised concern for being the primary etiology of tamponade, but resolution of symptoms and echocardiographic findings after thoracentesis clarified the source. This underscores the importance of considering alternative causes of tamponade physiology, particularly in postoperative cardiac patients with pleural effusion. Echocardiographic signs of tamponade are not specific to pericardial effusion; thus, clinical correlation and comprehensive imaging are essential to determine the true etiology. Timely recognition of pleural effusion-induced tamponade enables effective stabilization through a less invasive intervention and obviates unnecessary invasive cardiovascular procedures.
Conclusion:
Pleural effusion-induced tamponade is an uncommon but important pathology. Clinicians should maintain a broad differential when evaluating hemodynamic instability with echocardiographic signs of tamponade to ensure appropriate and targeted management.
Cardiac tamponade is a known hemodynamic complication of pericardial effusion. However, other less recognized etiologies can produce similar physiologic findings and require a distinct diagnostic and therapeutic approach. Accurate identification of the underlying cause of tamponade is essential for effective management.
Case Summary:
A 68-year-old woman, one month after bioprosthetic mitral valve replacement for severe mitral regurgitation, presented with fatigue and mild dyspnea on exertion. She was hypotensive and tachycardic, with pulsus paradoxus on exam. Transthoracic echocardiogram revealed a small anterior pericardial effusion and echocardiographic features consistent with tamponade physiology. A large right-sided pleural effusion was also discovered on CT imaging. She underwent urgent thoracentesis, after which tamponade findings resolved, and her symptoms markedly improved without pericardiocentesis.
Discussion:
This case highlights an uncommon but clinically significant cause of tamponade physiology: extracardiac compression from a large pleural effusion. While tamponade is usually due to pericardial fluid, elevated intrathoracic pressure from a pleural effusion can similarly impair diastolic filling and cause classic tamponade. The presence of a small pericardial effusion initially raised concern for being the primary etiology of tamponade, but resolution of symptoms and echocardiographic findings after thoracentesis clarified the source. This underscores the importance of considering alternative causes of tamponade physiology, particularly in postoperative cardiac patients with pleural effusion. Echocardiographic signs of tamponade are not specific to pericardial effusion; thus, clinical correlation and comprehensive imaging are essential to determine the true etiology. Timely recognition of pleural effusion-induced tamponade enables effective stabilization through a less invasive intervention and obviates unnecessary invasive cardiovascular procedures.
Conclusion:
Pleural effusion-induced tamponade is an uncommon but important pathology. Clinicians should maintain a broad differential when evaluating hemodynamic instability with echocardiographic signs of tamponade to ensure appropriate and targeted management.
More abstracts on this topic:
A Diagnosis Dilemma of Positional Hypoxia: Scoliosis-Mediated Platypnea-Orthodeoxia Syndrome
Ademuwagun Christianah, Arjoon Roy, Seth Paula, Chang Gene, Ibe Oby
A Community-Based Intervention to Improve Cardiovascular Health Understanding in the Dallas-Fort Worth South Asian CommunityDeo Parminder, Rohatgi Anand, Sharma Parul, Sathyamoorthy Mohanakrishnan