Final ID: Mo3135
Catastrophic Antiphospholipid Syndrome Mimicking Acute Coronary Syndrome: A Diagnostic Challenge with Critical Clinical Implications
Abstract Body (Do not enter title and authors here): Case Description:
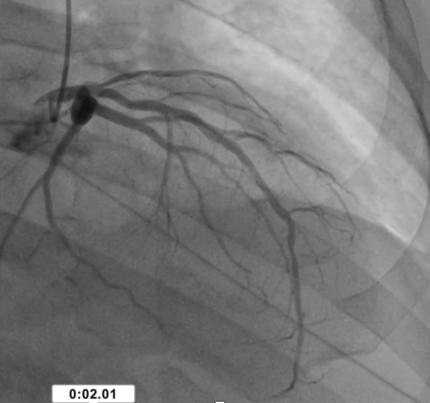
A 66-year-old male with a history of non-obstructive coronary artery disease [Image 1], unprovoked pulmonary embolism, hypertension, and diastolic heart failure presented with left-sided chest pressure three weeks post-NSTEMI. High-sensitivity troponin was elevated at 141 ng/L. He concurrently reported fingertip pain, intermittent confusion, and dizziness.
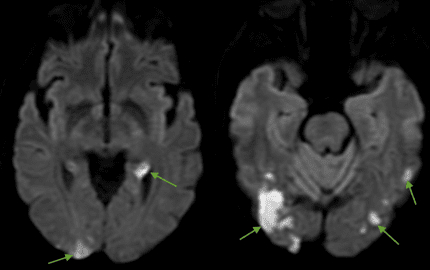
On hospital day two, he developed acute delirium, digital ischemia [Image 2], and right upper extremity pain. Brain MRI revealed multiple acute infarcts in bilateral frontoparietal, thalamic, and parieto-occipital territories [Image 3]. Despite therapeutic anticoagulation, a right upper extremity venous duplex showed acute brachial vein thrombosis. Anticoagulation was temporarily held, and warfarin was initiated due to suspected apixaban failure.
Laboratory workup revealed markedly elevated antiphospholipid antibodies (cardiolipin IgG >112 GPL, β2-glycoprotein I >112 SGU) and progressive thrombocytopenia (253K --> 91). Additional findings included retinal cotton wool spots and digital ischemia, confirming multi-organ involvement consistent with CAPS.
The patient was treated with combination “triple therapy” (therapeutic anticoagulation, high-dose steroids, and plasmapheresis), alongside rituximab, achieving clinical stabilization. Notably, failure of direct oral anticoagulant therapy reinforces the importance of using vitamin K antagonists in high-risk APS, consistent with current EULAR recommendations.
Discussion:
This case illustrates CAPS masquerading as recurrent ACS, with diagnostic ambiguity compounded by prior cardiac history and elevated troponins in the absence of coronary obstruction. Key red flags—including multi-territory infarcts, peripheral thromboses, and systemic signs—should prompt early evaluation for APS/CAPS. DOAC failure in this context adds to the growing evidence base against their use in high-risk APS patients. Warfarin remains the first-line therapy, particularly in triple-positive cases or those with recurrent thrombosis.
Key Takeaways:
1. Consider CAPS in patients with thrombotic events despite adequate anticoagulation.
2. Elevated troponins with non-obstructive coronary disease may reflect microvascular thrombosis.
3. Early recognition of multi-organ involvement is vital to prevent morbidity and mortality.
4. This case reinforces guideline-directed therapy with warfarin in high-risk APS/CAPS.
A 66-year-old male with a history of non-obstructive coronary artery disease [Image 1], unprovoked pulmonary embolism, hypertension, and diastolic heart failure presented with left-sided chest pressure three weeks post-NSTEMI. High-sensitivity troponin was elevated at 141 ng/L. He concurrently reported fingertip pain, intermittent confusion, and dizziness.
On hospital day two, he developed acute delirium, digital ischemia [Image 2], and right upper extremity pain. Brain MRI revealed multiple acute infarcts in bilateral frontoparietal, thalamic, and parieto-occipital territories [Image 3]. Despite therapeutic anticoagulation, a right upper extremity venous duplex showed acute brachial vein thrombosis. Anticoagulation was temporarily held, and warfarin was initiated due to suspected apixaban failure.
Laboratory workup revealed markedly elevated antiphospholipid antibodies (cardiolipin IgG >112 GPL, β2-glycoprotein I >112 SGU) and progressive thrombocytopenia (253K --> 91). Additional findings included retinal cotton wool spots and digital ischemia, confirming multi-organ involvement consistent with CAPS.
The patient was treated with combination “triple therapy” (therapeutic anticoagulation, high-dose steroids, and plasmapheresis), alongside rituximab, achieving clinical stabilization. Notably, failure of direct oral anticoagulant therapy reinforces the importance of using vitamin K antagonists in high-risk APS, consistent with current EULAR recommendations.
Discussion:
This case illustrates CAPS masquerading as recurrent ACS, with diagnostic ambiguity compounded by prior cardiac history and elevated troponins in the absence of coronary obstruction. Key red flags—including multi-territory infarcts, peripheral thromboses, and systemic signs—should prompt early evaluation for APS/CAPS. DOAC failure in this context adds to the growing evidence base against their use in high-risk APS patients. Warfarin remains the first-line therapy, particularly in triple-positive cases or those with recurrent thrombosis.
Key Takeaways:
1. Consider CAPS in patients with thrombotic events despite adequate anticoagulation.
2. Elevated troponins with non-obstructive coronary disease may reflect microvascular thrombosis.
3. Early recognition of multi-organ involvement is vital to prevent morbidity and mortality.
4. This case reinforces guideline-directed therapy with warfarin in high-risk APS/CAPS.
More abstracts on this topic:
Anticoagulant therapy for cerebral venous sinus thrombosis: A propensity score matching study
Liu Kai, Wei Zhao, Meng Zhang, Qin Dai, Song Bo, Xu Yuming
A Fecal-Derived Commensal Bacterium BM109 Reduces Infarct Size and Neurological Deficits in an Ischemic Stroke Rat ModelYoon Chung Eun, Kim You Bin, Nam Hyo Suk