Final ID: Su3142
Seconds to Save: Recognizing Type A Intramural Hematoma Before It’s Too Late
Abstract Body (Do not enter title and authors here): Case Presentation:
A 56-year-old woman with a history of hypertension and type 2 diabetes mellitus presented with acute, severe chest pain radiating to the back, which began while decorating her Christmas tree an hour prior to arrival. High-sensitivity troponin was elevated at 178 ng/L. Electrocardiogram revealed 1 mm horizontal ST elevations in the inferior leads without reciprocal changes. A triple-rule-out chest CT angiogram was obtained to evaluate for aortic dissection, pulmonary embolism, and coronary pathology. The scan showed no dissection, although contrast timing was optimized for pulmonary vasculature, limiting coronary and aortic detail. An ectatic ascending thoracic aorta (4.5 cm) was noted. Emergent left heart catheterization revealed mild, non-obstructive coronary artery disease.
Diagnostic Evaluation:
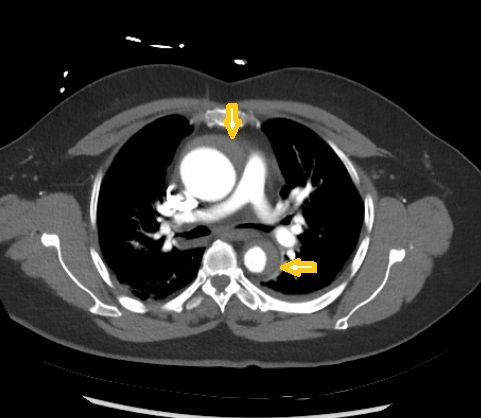
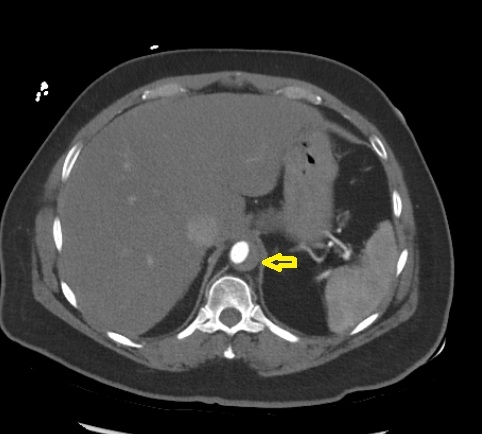
Given persistent suspicion for acute aortic syndrome, a dedicated CT angiogram of the aorta was performed, revealing an extensive intramural hematoma involving the aortic root, ascending aorta, arch, descending aorta, and abdominal aorta above the renal arteries.
Treatment and Management:
An esmolol infusion was initiated, and cardiothoracic surgery was urgently consulted. Imaging was interpreted as most consistent with a penetrating aortic ulcer and sub-adventitial hematoma. The patient underwent emergent surgical replacement of the ascending aorta and hemiarch. Intraoperative transesophageal echocardiogram did not reveal aortic regurgitation or pericardial effusion.
Discussion:
Intramural hematoma (IMH) is a form of acute aortic syndrome, with potential etiologies including rupture of vasa vasorum, neovascularization of atherosclerotic plaques, or microscopic intimal tears from penetrating ulcers. Prompt recognition is crucial, as IMH can mimic acute coronary syndrome (ACS) and misdiagnosis may result in harmful interventions. Tools such as the AORTAS score, which assigns two points for hypotension and one point each for aneurysm, pulse deficit, neurological deficit, severe pain, and sudden onset, can aid in risk stratification. A score >2, as in our patient (score = 3), warrants definitive imaging. Complications include hemopericardium, aortic regurgitation, and coronary compromise. Type A IMH mandates emergent surgical repair.
Conclusion:
A high index of suspicion is essential to differentiate IMH from ACS. Early, targeted imaging is critical, as interventions such as anticoagulation or invasive catheterization may accelerate disease progression.
A 56-year-old woman with a history of hypertension and type 2 diabetes mellitus presented with acute, severe chest pain radiating to the back, which began while decorating her Christmas tree an hour prior to arrival. High-sensitivity troponin was elevated at 178 ng/L. Electrocardiogram revealed 1 mm horizontal ST elevations in the inferior leads without reciprocal changes. A triple-rule-out chest CT angiogram was obtained to evaluate for aortic dissection, pulmonary embolism, and coronary pathology. The scan showed no dissection, although contrast timing was optimized for pulmonary vasculature, limiting coronary and aortic detail. An ectatic ascending thoracic aorta (4.5 cm) was noted. Emergent left heart catheterization revealed mild, non-obstructive coronary artery disease.
Diagnostic Evaluation:
Given persistent suspicion for acute aortic syndrome, a dedicated CT angiogram of the aorta was performed, revealing an extensive intramural hematoma involving the aortic root, ascending aorta, arch, descending aorta, and abdominal aorta above the renal arteries.
Treatment and Management:
An esmolol infusion was initiated, and cardiothoracic surgery was urgently consulted. Imaging was interpreted as most consistent with a penetrating aortic ulcer and sub-adventitial hematoma. The patient underwent emergent surgical replacement of the ascending aorta and hemiarch. Intraoperative transesophageal echocardiogram did not reveal aortic regurgitation or pericardial effusion.
Discussion:
Intramural hematoma (IMH) is a form of acute aortic syndrome, with potential etiologies including rupture of vasa vasorum, neovascularization of atherosclerotic plaques, or microscopic intimal tears from penetrating ulcers. Prompt recognition is crucial, as IMH can mimic acute coronary syndrome (ACS) and misdiagnosis may result in harmful interventions. Tools such as the AORTAS score, which assigns two points for hypotension and one point each for aneurysm, pulse deficit, neurological deficit, severe pain, and sudden onset, can aid in risk stratification. A score >2, as in our patient (score = 3), warrants definitive imaging. Complications include hemopericardium, aortic regurgitation, and coronary compromise. Type A IMH mandates emergent surgical repair.
Conclusion:
A high index of suspicion is essential to differentiate IMH from ACS. Early, targeted imaging is critical, as interventions such as anticoagulation or invasive catheterization may accelerate disease progression.
More abstracts on this topic:
Apolipoprotein A2 as Protection Against Increased Mortality After Aortic Aneurysm Repair
Eguchi Miu, Nakamura Takamitsu, Omori Kazuhira, Horikoshi Takeo, Yoshizaki Toru, Kobayashi Tsuyoshi, Sato Akira
CC-Chemokine Receptor 2 Inhibition Prevents Monocyte/Macrophages Recruitment in Abdominal Aortic AneurysmsElizondo Benedetto Santiago, Zaghloul Mohamed, Arif Batool, Bredemeyer Andrea, Lavine Kory, Gropler Robert, Liu Yongjian, Zayed Mohamed