Final ID: MP1983
Disparities in Percutaneous Coronary Intervention and Outcomes Among Patients With and Without Dementia Hospitalized for Acute Coronary Syndrome: A Nationwide Propensity Score–Matched Analysis
Abstract Body (Do not enter title and authors here): Introduction
Older age and multimorbidity observed in individuals with dementia may impact both the care they receive and their outcomes in the setting of acute coronary syndrome (ACS). We conducted an analysis of ACS hospitalizations in the US to examine whether disparities exist between patients with and without dementia in percutaneous coronary intervention (PCI) use and ACS-related outcomes after accounting for age and comorbidities.
Methods
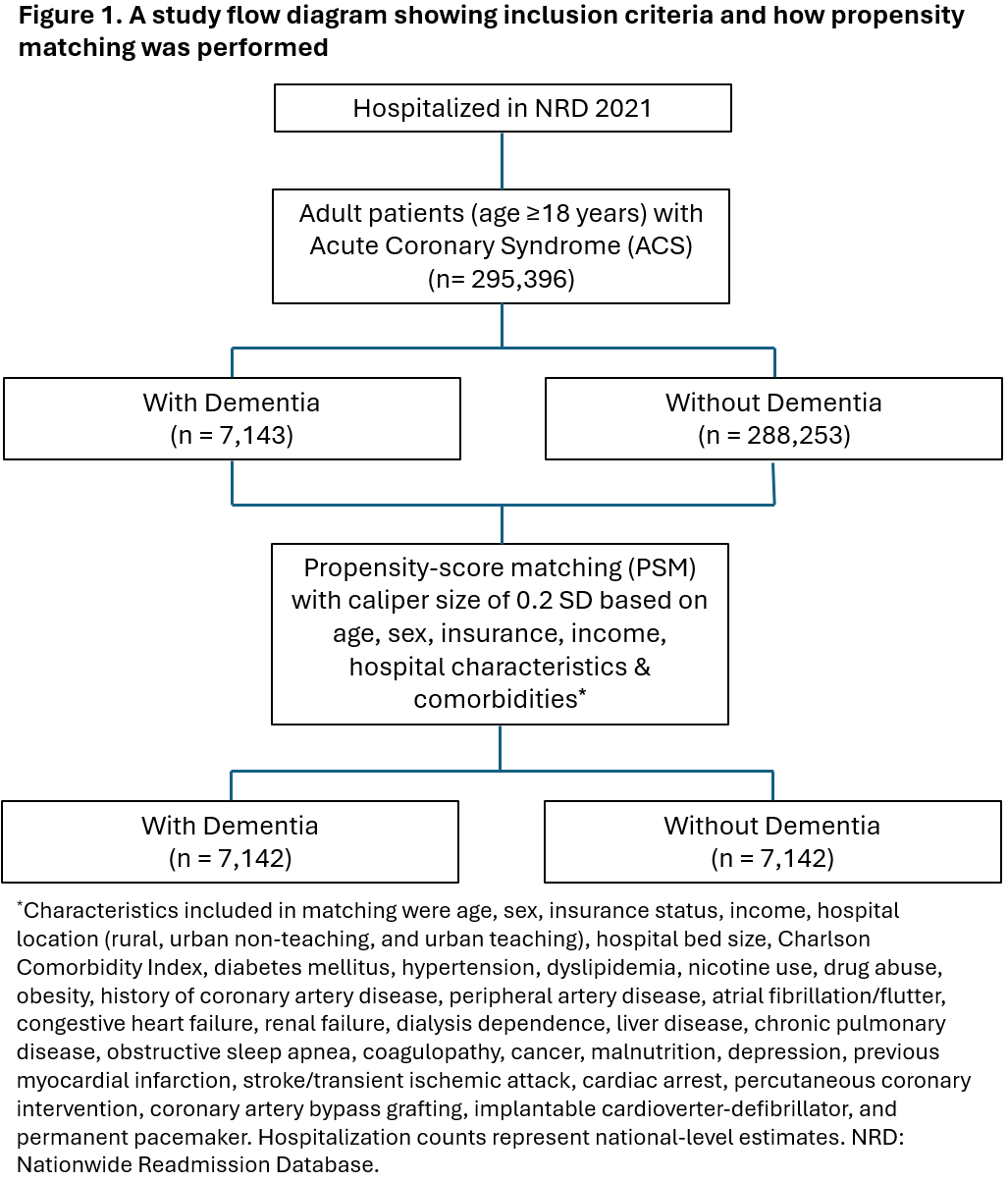
We used the Nationwide Readmissions Database 2021 to identify adults hospitalized with a primary diagnosis of ACS, including STEMI and NSTEMI. Propensity scores for dementia were calculated using 33 baseline characteristics, including age, sex, insurance, income, hospital characteristics, Charlson comorbidity index, and other relevant comorbidities. We performed 1:1 nearest-neighbor matching with a caliper of 0.2 standard deviations. After matching, we compare the following outcomes of people with and without dementia: receipt of PCI, mechanical complications of ACS, cardiogenic shock, mechanical circulatory support, inpatient mortality, length of stay, and hospitalization cost, and reported odds ratios or mean difference, 95% confidence interval, p-value. Survey weights were applied to ensure national representativeness.
Results
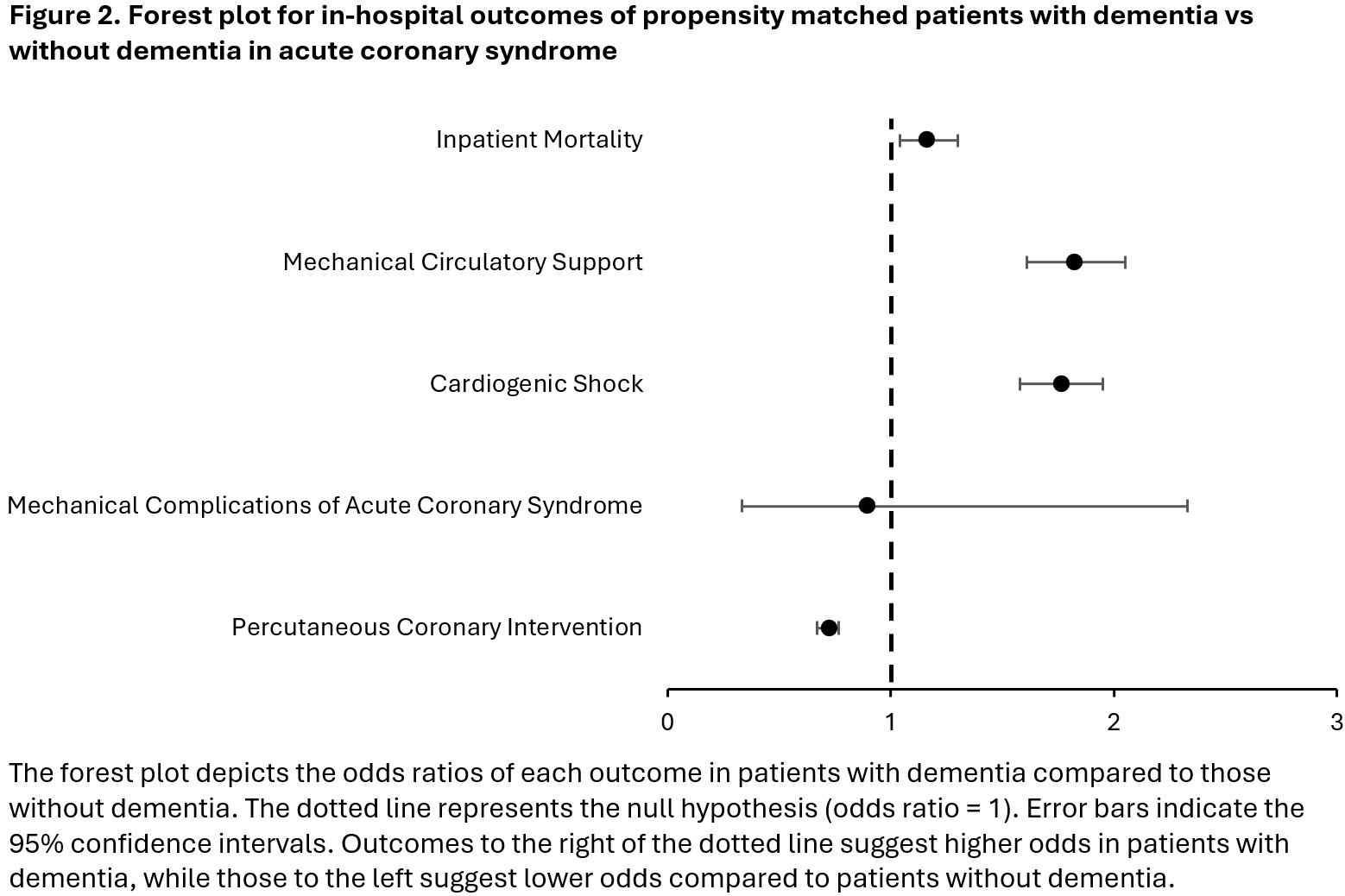
Among 295,396 patients hospitalized with ACS, 7,143 had dementia. After matching, 7,142 patients with and without dementia were identified for analysis (Figure 1). Covariate balance was achieved (all standardized mean differences <.1). Patients with dementia were 28% less likely to undergo PCI (0.72 [0.67–0.77], p<.001) and 78% more likely to develop cardiogenic shock (1.76 [1.58–1.95], p<.001), 82% more likely to require mechanical circulatory support (1.82 [1.61–2.05], p<.001), and 16% more likely to die during hospitalization (1.16 [1.04–1.30], p<.01) (Figure 2). No significant difference was observed in mechanical complications of ACS (0.89 [0.33–2.33], p=.81). Patients with dementia had longer hospital stays (9.27 vs. 5.89 days; mean difference 3.38 [3.06-3.7] days, p<.001) and higher hospitalization costs ($182,649 vs. $130,233; mean difference $52,416 [$44,618- $60,215], p<.001).
Conclusion
In this analysis of US hospitalizations for ACS, dementia was independently associated with lower PCI rates and worse ACS-related outcomes despite accounting for age and comorbidities. Further research is needed to understand and address these inequities in ACS management in patients with dementia.
Older age and multimorbidity observed in individuals with dementia may impact both the care they receive and their outcomes in the setting of acute coronary syndrome (ACS). We conducted an analysis of ACS hospitalizations in the US to examine whether disparities exist between patients with and without dementia in percutaneous coronary intervention (PCI) use and ACS-related outcomes after accounting for age and comorbidities.
Methods
We used the Nationwide Readmissions Database 2021 to identify adults hospitalized with a primary diagnosis of ACS, including STEMI and NSTEMI. Propensity scores for dementia were calculated using 33 baseline characteristics, including age, sex, insurance, income, hospital characteristics, Charlson comorbidity index, and other relevant comorbidities. We performed 1:1 nearest-neighbor matching with a caliper of 0.2 standard deviations. After matching, we compare the following outcomes of people with and without dementia: receipt of PCI, mechanical complications of ACS, cardiogenic shock, mechanical circulatory support, inpatient mortality, length of stay, and hospitalization cost, and reported odds ratios or mean difference, 95% confidence interval, p-value. Survey weights were applied to ensure national representativeness.
Results
Among 295,396 patients hospitalized with ACS, 7,143 had dementia. After matching, 7,142 patients with and without dementia were identified for analysis (Figure 1). Covariate balance was achieved (all standardized mean differences <.1). Patients with dementia were 28% less likely to undergo PCI (0.72 [0.67–0.77], p<.001) and 78% more likely to develop cardiogenic shock (1.76 [1.58–1.95], p<.001), 82% more likely to require mechanical circulatory support (1.82 [1.61–2.05], p<.001), and 16% more likely to die during hospitalization (1.16 [1.04–1.30], p<.01) (Figure 2). No significant difference was observed in mechanical complications of ACS (0.89 [0.33–2.33], p=.81). Patients with dementia had longer hospital stays (9.27 vs. 5.89 days; mean difference 3.38 [3.06-3.7] days, p<.001) and higher hospitalization costs ($182,649 vs. $130,233; mean difference $52,416 [$44,618- $60,215], p<.001).
Conclusion
In this analysis of US hospitalizations for ACS, dementia was independently associated with lower PCI rates and worse ACS-related outcomes despite accounting for age and comorbidities. Further research is needed to understand and address these inequities in ACS management in patients with dementia.
More abstracts on this topic:
10-Year Trends in Last Known Well to Arrival Time in Acute Ischemic Stroke Patients: 2014-2023
Ferrone Nicholas, Sanmartin Maria, O'hara Joseph, Jimenez Jean, Ferrone Sophia, Wang Jason, Katz Jeffrey, Sanelli Pina
A Polypill Strategy for Heart Failure with Reduced Ejection Fraction: The POLY-HF TrialPandey Ambarish, Wang Thomas, Keshvani Neil, Rizvi Syed Kazim, Jain Anand, Coellar Juan David, Drazner Mark, Gupta Deepak, Chandra Alvin, Zaha Vlad