Final ID: Sa3061
Oral Anticoagulant Monotherapy vs Dual Antithrombotic Therapy in Patients with Atrial Fibrillation and Stable Coronary Artery Disease Following Percutaneous Coronary Intervention: Insights from a Real-World TriNetX Cohort Study
Abstract Body (Do not enter title and authors here): Background:
The optimal long-term antithrombotic strategy in patients with atrial fibrillation (AF) and stable coronary artery disease (CAD) post-percutaneous coronary intervention (PCI) remains uncertain. While oral anticoagulant (OAC) monotherapy may reduce bleeding risk, concerns persist regarding its effectiveness in preventing ischemic events compared to combined OAC and single antiplatelet therapy (SAPT).
Aim:
This study aimed to compare the effectiveness and safety of OAC monotherapy versus combined OAC and SAPT in a real-world cohort of patients with AF and stable CAD, ≥1 year post-PCI.
Methods:
Using the TriNetX global federated health research network, we conducted a retrospective cohort analysis including 6,950 matched patients on OAC monotherapy and 6,950 matched patients on combined OAC and SAPT, after propensity score matching from initial cohorts of 10,304 and 8,235 patients, respectively. Outcomes evaluated at 1 and 3 years included all-cause mortality, ischemic stroke, myocardial infarction (MI), pulmonary embolism (PE), and major bleeding events.
Results:
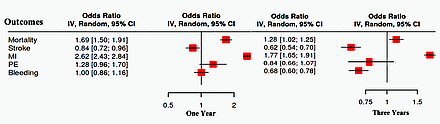
At 1 year, OAC monotherapy had higher mortality (10.8% vs. 6.7%; OR 1.690, CI [1.497,1.907], p<0.001), lower stroke risk (5.4% vs. 6.4%; OR 0.835, CI [0.725,0.963], p=0.013), higher MI (36.2% vs. 17.8%; OR 2.624, CI [2.426,2.839], p<0.001), with no difference in PE (1.6% vs. 1.3%; OR 1.2, CI [0.965,1.699], p=0.086) or bleeding (5.3% each; OR 1.0, CI [0.862,1.161], p=1.0). At 3 years, OAC monotherapy demonstrated sustained higher mortality (13.6% vs. 12.3%; OR 1.128, CI [1.021,1.245], p=0.018), higher MI (36.7% vs. 24.6%; OR 1.772, CI [1.647,1.907], p<0.001), reduced stroke risk (5.8% vs. 9.1%; OR 0.617, CI [0.542,0.702], p<0.001), and lower bleeding (6.0% vs. 8.5%; OR 0.683, CI [0.600,0.778], p<0.001), with no difference in PE.
Conclusions:
In this large, real-world matched cohort, OAC monotherapy in patients with AF and stable CAD post-PCI was associated with increased mortality and significantly higher myocardial infarction rates despite a reduction in ischemic stroke compared to combined therapy. OAC monotherapy was associated with significantly lower bleeding risk at 3 years.
The optimal long-term antithrombotic strategy in patients with atrial fibrillation (AF) and stable coronary artery disease (CAD) post-percutaneous coronary intervention (PCI) remains uncertain. While oral anticoagulant (OAC) monotherapy may reduce bleeding risk, concerns persist regarding its effectiveness in preventing ischemic events compared to combined OAC and single antiplatelet therapy (SAPT).
Aim:
This study aimed to compare the effectiveness and safety of OAC monotherapy versus combined OAC and SAPT in a real-world cohort of patients with AF and stable CAD, ≥1 year post-PCI.
Methods:
Using the TriNetX global federated health research network, we conducted a retrospective cohort analysis including 6,950 matched patients on OAC monotherapy and 6,950 matched patients on combined OAC and SAPT, after propensity score matching from initial cohorts of 10,304 and 8,235 patients, respectively. Outcomes evaluated at 1 and 3 years included all-cause mortality, ischemic stroke, myocardial infarction (MI), pulmonary embolism (PE), and major bleeding events.
Results:
At 1 year, OAC monotherapy had higher mortality (10.8% vs. 6.7%; OR 1.690, CI [1.497,1.907], p<0.001), lower stroke risk (5.4% vs. 6.4%; OR 0.835, CI [0.725,0.963], p=0.013), higher MI (36.2% vs. 17.8%; OR 2.624, CI [2.426,2.839], p<0.001), with no difference in PE (1.6% vs. 1.3%; OR 1.2, CI [0.965,1.699], p=0.086) or bleeding (5.3% each; OR 1.0, CI [0.862,1.161], p=1.0). At 3 years, OAC monotherapy demonstrated sustained higher mortality (13.6% vs. 12.3%; OR 1.128, CI [1.021,1.245], p=0.018), higher MI (36.7% vs. 24.6%; OR 1.772, CI [1.647,1.907], p<0.001), reduced stroke risk (5.8% vs. 9.1%; OR 0.617, CI [0.542,0.702], p<0.001), and lower bleeding (6.0% vs. 8.5%; OR 0.683, CI [0.600,0.778], p<0.001), with no difference in PE.
Conclusions:
In this large, real-world matched cohort, OAC monotherapy in patients with AF and stable CAD post-PCI was associated with increased mortality and significantly higher myocardial infarction rates despite a reduction in ischemic stroke compared to combined therapy. OAC monotherapy was associated with significantly lower bleeding risk at 3 years.
More abstracts on this topic:
12,13-diHOME Attenuates Pro-Arrhythmic Effect of High-Fat Diet
Acute Myocardial Infarction outcomes in patients on single anticoagulation versus combined anticoagulation and antiplatelet therapy
Buck Benjamin, Baer Lisa, Deschenes Isabelle, Chinthalapudi Krishna, Gallego-perez Daniel, Stanford Kristin, Hund Thomas, Areiza Natalia, Xu Xianyao, Elliott Austin, Wan Xiaoping, Nassal Drew, Lane Cemantha, Nirengi Shinsuke, James Natasha Maria
Acute Myocardial Infarction outcomes in patients on single anticoagulation versus combined anticoagulation and antiplatelet therapy
Rosario Manuel, Vasquez Moises, Garcia Gustavo, Wojtas Caroline, Vargas Ian, Behers Benjamin