Final ID: Sa2076
High Catastrophic Spending Among Younger Patients with CVD or Related Risk Factors
Abstract Body (Do not enter title and authors here):
Introduction/Background: Since 2010, there has been an increase in cardiovascular disease (CVD) mortality among younger adults aged 25-64 years. There is growing concern that financial barriers in accessing health care services may be contributing to these concerning trends, particularly among privately-insured adults with cardiometabolic risk factors and/or established cardiovascular disease, who face increasing copayments and deductibles. Understanding whether health expenditures and financial burden have worsened for those with CVD or related risk factors has important implications for both patients and policymakers.
Research Question: This study aimed to understand how total health care costs, including patient-contributions to insurance premiums and out-of-pocket costs for medical and prescription drug care, changed among adults aged 25 to 64 years with CVD (defined as coronary artery disease, angina pectoris, heart attack, or stroke) and/or related risk factors (hypertension, diabetes, hyperlipidemia, peripheral artery disease, or transient ischemic attacks). In addition, we determined changes in the financial burden of health care (defined as health care expenditures divided by income) and catastrophic health spending (defined as spending over 10% of income on health expenditures).
Methods: Using the Medical Expenditure Panel Survey (MEPS) public use files from 2007-2022, we fit survey-weighted regression models to evaluate changes in outcomes. National projections were estimated using survey weights. We estimated inflation-adjusted dollar values to 2022 US dollars.
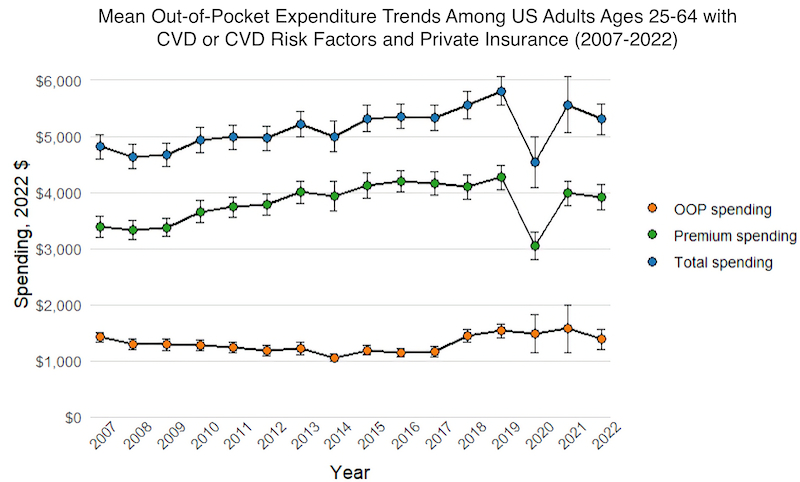
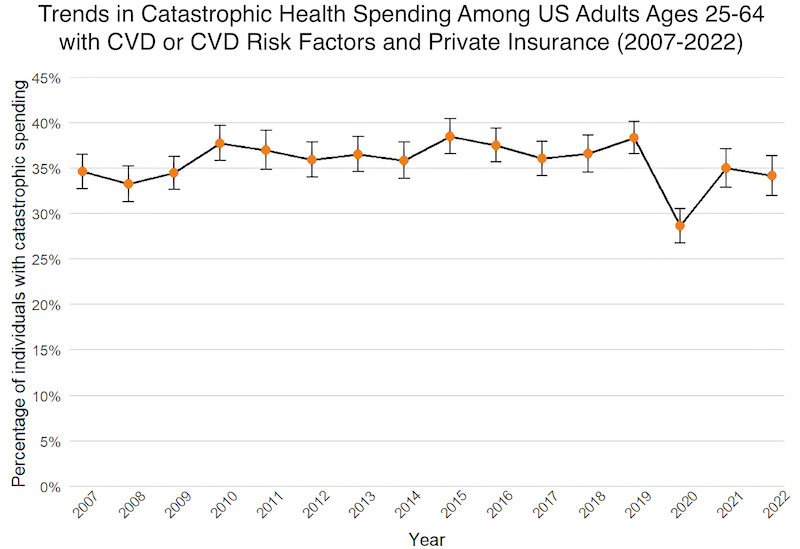
Results: Between 2007 and 2022, total health care expenditures for patients with CVD or risk factors increased from $4813 (95% CI: $4597, $5030) to $5304 (95% CI: $5030, $5577). This rise was largely driven by an increase in premiums ($3389 [$3196, 3582] to $3919 [$3698, $4141]), while out-of-pocket costs for medical care and prescription drugs were largely stable ($1424 [$1335, $1514] to $1384 [$1210, $1558]). While financial burden mildly decreased from 16.4% [15.5%, 17.4%] to 14.8% [13.8%, 15.8%] over this period, catastrophic health spending did not improve (34.6% [32.7%, 36.5%] to 34.2% [32.0%, 36.4%]).
Conclusion: In this national study of younger adults with CVD or related risk factors, total health care costs increased, driven largely by a rise in insurance premiums. In addition, the burden of catastrophic health care spending remains high in this population.
Introduction/Background: Since 2010, there has been an increase in cardiovascular disease (CVD) mortality among younger adults aged 25-64 years. There is growing concern that financial barriers in accessing health care services may be contributing to these concerning trends, particularly among privately-insured adults with cardiometabolic risk factors and/or established cardiovascular disease, who face increasing copayments and deductibles. Understanding whether health expenditures and financial burden have worsened for those with CVD or related risk factors has important implications for both patients and policymakers.
Research Question: This study aimed to understand how total health care costs, including patient-contributions to insurance premiums and out-of-pocket costs for medical and prescription drug care, changed among adults aged 25 to 64 years with CVD (defined as coronary artery disease, angina pectoris, heart attack, or stroke) and/or related risk factors (hypertension, diabetes, hyperlipidemia, peripheral artery disease, or transient ischemic attacks). In addition, we determined changes in the financial burden of health care (defined as health care expenditures divided by income) and catastrophic health spending (defined as spending over 10% of income on health expenditures).
Methods: Using the Medical Expenditure Panel Survey (MEPS) public use files from 2007-2022, we fit survey-weighted regression models to evaluate changes in outcomes. National projections were estimated using survey weights. We estimated inflation-adjusted dollar values to 2022 US dollars.
Results: Between 2007 and 2022, total health care expenditures for patients with CVD or risk factors increased from $4813 (95% CI: $4597, $5030) to $5304 (95% CI: $5030, $5577). This rise was largely driven by an increase in premiums ($3389 [$3196, 3582] to $3919 [$3698, $4141]), while out-of-pocket costs for medical care and prescription drugs were largely stable ($1424 [$1335, $1514] to $1384 [$1210, $1558]). While financial burden mildly decreased from 16.4% [15.5%, 17.4%] to 14.8% [13.8%, 15.8%] over this period, catastrophic health spending did not improve (34.6% [32.7%, 36.5%] to 34.2% [32.0%, 36.4%]).
Conclusion: In this national study of younger adults with CVD or related risk factors, total health care costs increased, driven largely by a rise in insurance premiums. In addition, the burden of catastrophic health care spending remains high in this population.
More abstracts on this topic:
A Measure of Residential Segregation and Thrombo-inflammation in Black and White Americans
Manogaran Erin, Cushman Mary, Kamin Mukaz Debora, Sparks Andrew, Packer Ryan, Brochu Paige, Judd Suzanne, Howard Virginia, Plante Timothy, Long Leann, Cheung Katherine
An Examination of LGBT Non-Discrimination Laws and CVD Risk Among US VeteransDuncan Meredith, Goulet Joseph, Oleary John, Skanderson Melissa, Streed Carl