Final ID: MDP1542
Medicaid Work Requirements and Changes in Insurance Coverage, Employment, Access to Care, and Health Status Overall and Among People with Cardiovascular Disease
Abstract Body (Do not enter title and authors here): Introduction: Medicaid work requirements have been at the forefront of health policy debate. Proponents argue that these policies increase employment, reduce poverty, and improve health. Critics have raised concerns that work requirements lead to loss of coverage and impede access to care.
Hypothesis: We hypothesized that Medicaid work requirement implementation would be associated with decreased insurance coverage and healthcare access without impacting employment.
Methods: We used the Behavioral Risk Factor Surveillance System (a nationally representative survey administered by the CDC) to estimate the impact of Medicaid work requirements on insurance coverage, employment, access to care, and self-reported health. We used a difference-in-differences (DID) approach to compare changes in outcomes in Arkansas (where work requirements were implemented) versus control states. Outcomes were self-reported and included: 1) insurance coverage, 2) employment, 3) presence of a personal healthcare provider, 4) inability to see a doctor due to cost, and 5) self-reported health. The analysis was conducted among all respondents and among respondents with cardiovascular disease, who were hypothesized to be particularly vulnerable to negative sequelae of insurance loss.
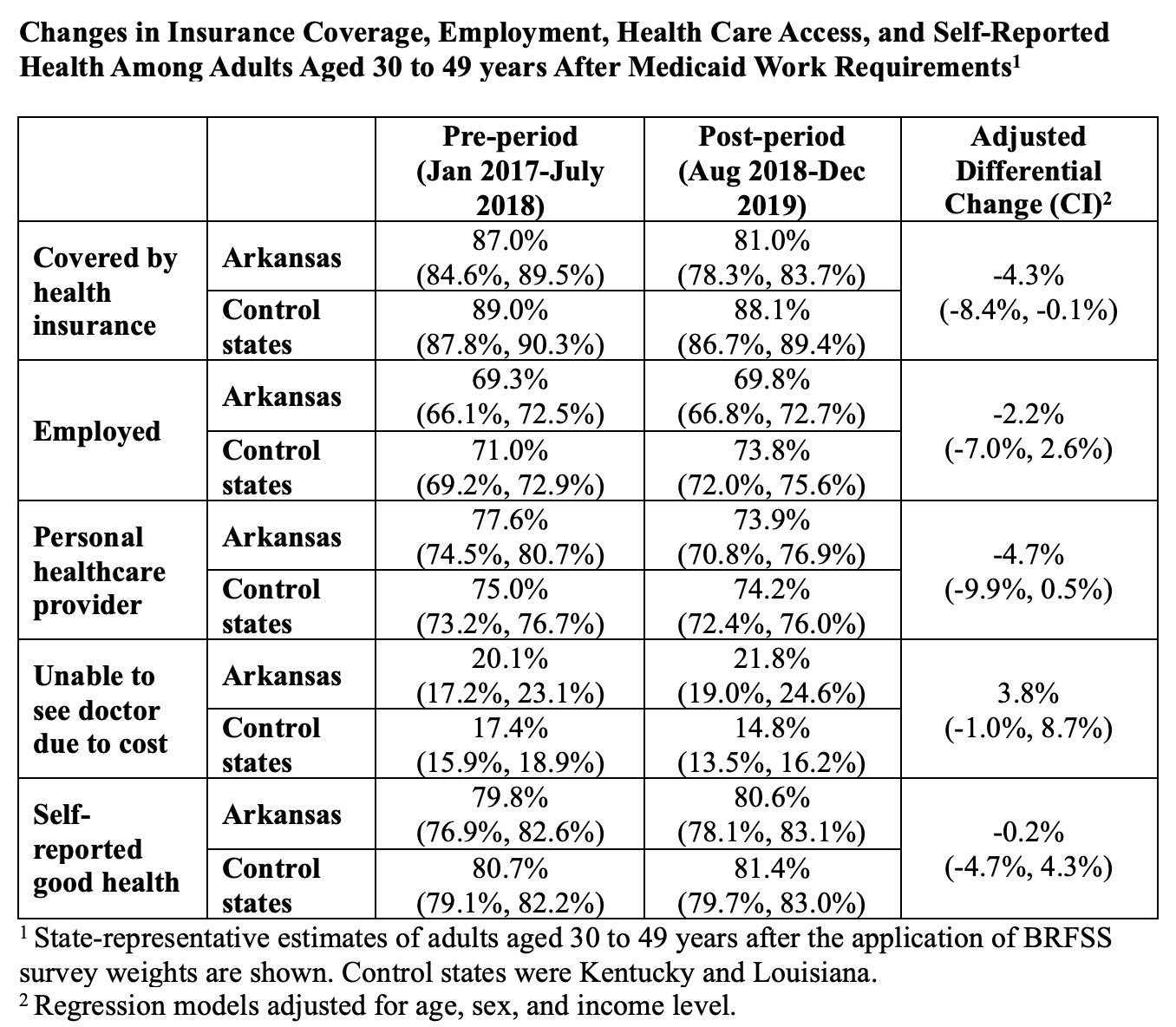
Results: The implementation of Medicaid work requirements in Arkansas was associated with decreased insurance coverage compared with control states (adjusted DID estimate -4.3%, CI -8.4%, -0.1%), but no increase in employment rates (-2.2% CI -7.0%, 2.6%). There was a trend toward decreased likelihood of having a personal healthcare provider (-4.7% CI -9.9%, 0.5%). There was no change in inability to see a doctor due to cost or self-reported good health. When this analysis was repeated among participants with cardiovascular disease, work requirement implementation was not associated with changes in any of the outcome variables.
Conclusions: The implementation of Medicaid work requirements in Arkansas was associated with decreased insurance coverage and no change in employment. Our findings are particularly relevant given national policy debate about work requirement expansion and the recent implementation of Medicaid work requirements in Georgia. Despite the null findings among respondents with cardiovascular disease (likely the result of a small sample size), this study has important implications for cardiovascular health given the close association between insurance coverage and cardiovascular outcomes.
Hypothesis: We hypothesized that Medicaid work requirement implementation would be associated with decreased insurance coverage and healthcare access without impacting employment.
Methods: We used the Behavioral Risk Factor Surveillance System (a nationally representative survey administered by the CDC) to estimate the impact of Medicaid work requirements on insurance coverage, employment, access to care, and self-reported health. We used a difference-in-differences (DID) approach to compare changes in outcomes in Arkansas (where work requirements were implemented) versus control states. Outcomes were self-reported and included: 1) insurance coverage, 2) employment, 3) presence of a personal healthcare provider, 4) inability to see a doctor due to cost, and 5) self-reported health. The analysis was conducted among all respondents and among respondents with cardiovascular disease, who were hypothesized to be particularly vulnerable to negative sequelae of insurance loss.
Results: The implementation of Medicaid work requirements in Arkansas was associated with decreased insurance coverage compared with control states (adjusted DID estimate -4.3%, CI -8.4%, -0.1%), but no increase in employment rates (-2.2% CI -7.0%, 2.6%). There was a trend toward decreased likelihood of having a personal healthcare provider (-4.7% CI -9.9%, 0.5%). There was no change in inability to see a doctor due to cost or self-reported good health. When this analysis was repeated among participants with cardiovascular disease, work requirement implementation was not associated with changes in any of the outcome variables.
Conclusions: The implementation of Medicaid work requirements in Arkansas was associated with decreased insurance coverage and no change in employment. Our findings are particularly relevant given national policy debate about work requirement expansion and the recent implementation of Medicaid work requirements in Georgia. Despite the null findings among respondents with cardiovascular disease (likely the result of a small sample size), this study has important implications for cardiovascular health given the close association between insurance coverage and cardiovascular outcomes.
More abstracts on this topic:
A Community Outreach Program Focused on Hypertension Awareness Reaches 600+ People in Rural Georgia and Works to Build the Next Generation of Biomedical Scientists
Dent Elena, Ilatovskaya Daria, Pinkerton Brittany, Crider Emily, Ryan Michael, Sullivan Jennifer
3-Minute Heart Health App: A Feasibility StudyAbdulkarim Iya, Metzger Joseph, Stovitz Steven, Van't Hof Jeremy