Final ID: MP1799
Acute Inferolateral STEMI as an Initial Presentation of Polycythemia Vera with Recurrent Coronary Thrombosis Despite Triple Therapy
Abstract Body (Do not enter title and authors here): Case
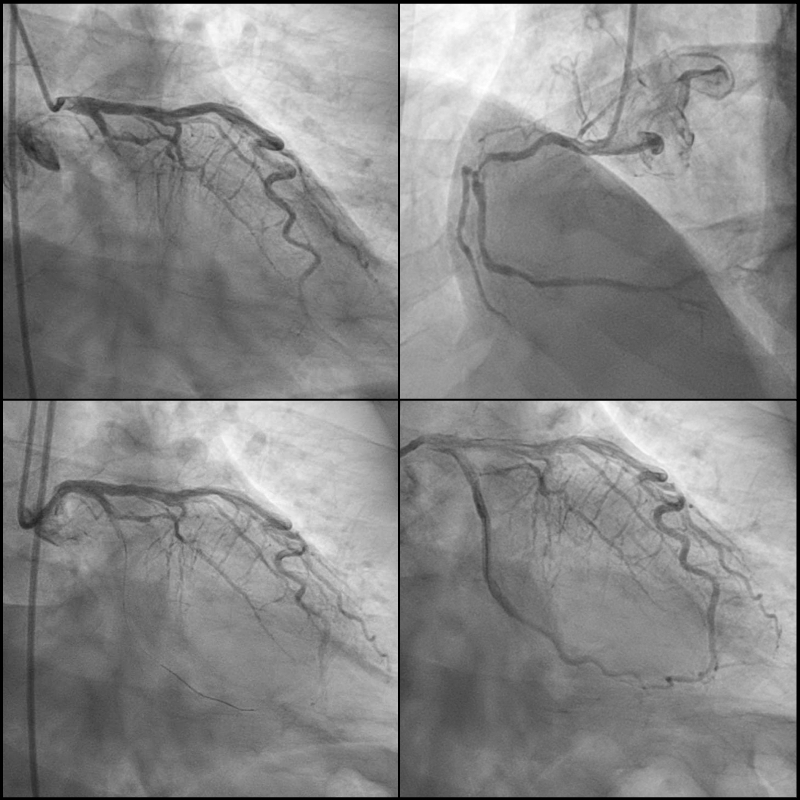
A 60-year-old man with history of hypertension, diabetes, and remote history of unprovoked lower extremity DVT presented with dyspnea for 3 days and chest pain for 1 day. Initial ECG revealed acute inferolateral STEMI (Figure 1A). Initial labs showed marked polycythemia (hemoglobin 21.6 g/dL, hematocrit 65%). Emergent coronary angiogram (CAG) demonstrated 100% occlusion of the LCx (Figure 2), where PCI with 4 drug-eluting stents (DES) was performed. There was residual 85% stenosis of the RCA. Echocardiogram showed ejection fraction (EF) 45% with severe hypokinesis of the inferolateral wall. Patient was started on aspirin, prasugrel, and rosuvastatin. Given his polycythemia and history of DVT, hematology was consulted and started apixaban for secondary thromboprophylaxis with no indication of phlebotomy in the setting of recent STEMI. JAK2 V617F mutation positive confirmed the diagnosis of polycythemia vera (PV). Hospital course was complicated by worsening renal function, likely due to contrast-induced nephropathy and/or cholesterol emboli.
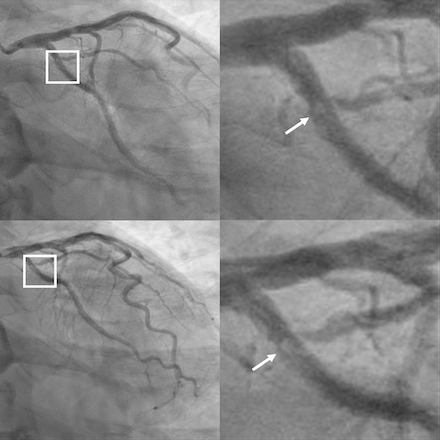
One week later, he developed acute epigastric pain and hypotension requiring vasopressors. Despite triple therapy (aspirin, prasugrel, apixaban), ECG indicated lateral STEMI (Figure 1B). Repeated CAG showed a new thrombus in the proximal LCx stents though there was TIMI 3 flow (Figure 3). Aspiration thrombectomy with 2 additional DES were placed. Right heart catheterization revealed mixed cardiogenic and vasoplegic shock, most likely from metabolic acidosis and uremia. A temporary ventricular support device was inserted, and CRRT was started. Repeated echocardiogram showed EF 30%. Patient subsequently developed DIC and multiorgan failure. Despite maximal support, he developed coffee ground emesis which was likely aspirated leading to PEA cardiac arrest.
Discussion
This case highlights the increased thrombotic risk in patients with PV, with JAK2 mutation as a known important contributor to a hypercoagulable state, leading to recurrent coronary thrombosis despite triple therapy. High-risk PV, characterized by JAK2 mutation, prior thrombosis, and age over 60, all of which were present in this case, is associated with significant risk of both arterial and venous thrombotic events. Prompt recognition and management of PV are critical. Early hematology involvement and initiation of cytoreductive measures, such as phlebotomy and hydroxyurea, to keep hematocrit <45% could reduce the risk of recurrent thrombotic events.
A 60-year-old man with history of hypertension, diabetes, and remote history of unprovoked lower extremity DVT presented with dyspnea for 3 days and chest pain for 1 day. Initial ECG revealed acute inferolateral STEMI (Figure 1A). Initial labs showed marked polycythemia (hemoglobin 21.6 g/dL, hematocrit 65%). Emergent coronary angiogram (CAG) demonstrated 100% occlusion of the LCx (Figure 2), where PCI with 4 drug-eluting stents (DES) was performed. There was residual 85% stenosis of the RCA. Echocardiogram showed ejection fraction (EF) 45% with severe hypokinesis of the inferolateral wall. Patient was started on aspirin, prasugrel, and rosuvastatin. Given his polycythemia and history of DVT, hematology was consulted and started apixaban for secondary thromboprophylaxis with no indication of phlebotomy in the setting of recent STEMI. JAK2 V617F mutation positive confirmed the diagnosis of polycythemia vera (PV). Hospital course was complicated by worsening renal function, likely due to contrast-induced nephropathy and/or cholesterol emboli.
One week later, he developed acute epigastric pain and hypotension requiring vasopressors. Despite triple therapy (aspirin, prasugrel, apixaban), ECG indicated lateral STEMI (Figure 1B). Repeated CAG showed a new thrombus in the proximal LCx stents though there was TIMI 3 flow (Figure 3). Aspiration thrombectomy with 2 additional DES were placed. Right heart catheterization revealed mixed cardiogenic and vasoplegic shock, most likely from metabolic acidosis and uremia. A temporary ventricular support device was inserted, and CRRT was started. Repeated echocardiogram showed EF 30%. Patient subsequently developed DIC and multiorgan failure. Despite maximal support, he developed coffee ground emesis which was likely aspirated leading to PEA cardiac arrest.
Discussion
This case highlights the increased thrombotic risk in patients with PV, with JAK2 mutation as a known important contributor to a hypercoagulable state, leading to recurrent coronary thrombosis despite triple therapy. High-risk PV, characterized by JAK2 mutation, prior thrombosis, and age over 60, all of which were present in this case, is associated with significant risk of both arterial and venous thrombotic events. Prompt recognition and management of PV are critical. Early hematology involvement and initiation of cytoreductive measures, such as phlebotomy and hydroxyurea, to keep hematocrit <45% could reduce the risk of recurrent thrombotic events.
More abstracts on this topic:
A New Analytical Approach for Noninvasive Reconstruction of the Entire Left Ventricular Pressure Waveform in Myocardial Ischemia and Infarction
Bilgi Coskun, Li Jiajun, Alavi Rashid, Dai Wangde, Matthews Ray, Kloner Robert, Pahlevan Niema
Acute Left Ventricular Thrombosis and Systemic Embolism Following Testosterone TherapyRasheed Ahmed Daniyaal, Naseer Ahmed, Nadig Vidya