Final ID: MP1801
Conservative Management of Non-Obstructive Left Main Coronary Artery Thrombus in the Setting of Myopericarditis
Abstract Body (Do not enter title and authors here): Background:
Left main (LM) coronary artery thrombus is a rare but life-threatening condition, typically associated with acute coronary syndromes requiring urgent intervention. Certain conditions such as myopericarditis contribute to a prothrombotic state through systemic inflammation. In rare cases, this may predispose to coronary thrombosis, particularly in patients with additional risk factors. We describe a case in which myopericarditis likely contributed to the formation of a non-obstructive left main coronary artery thrombus in the setting of overlapping systemic inflammation and underlying prothrombotic risk, managed conservatively without percutaneous intervention.
Case presentation:
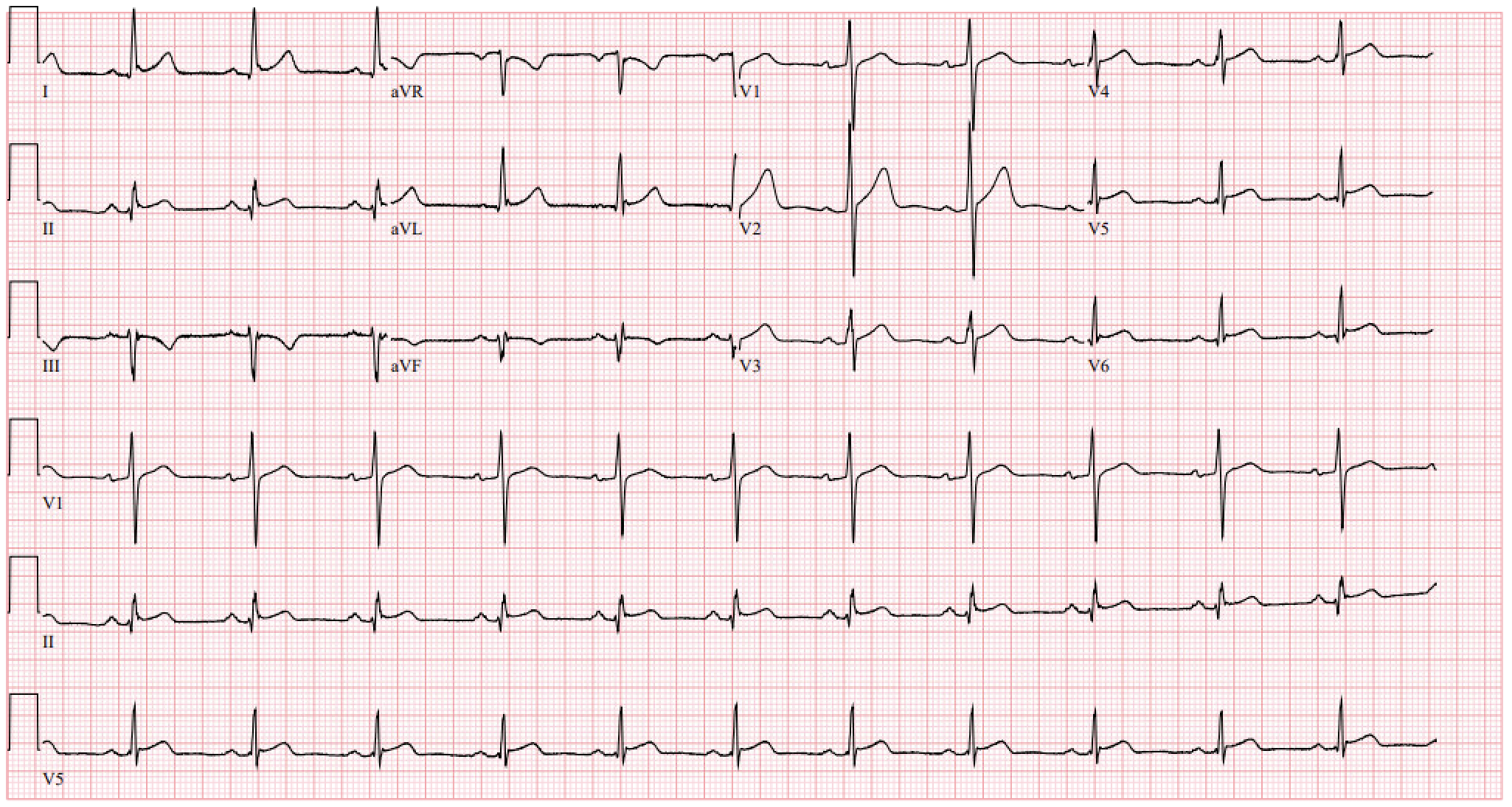
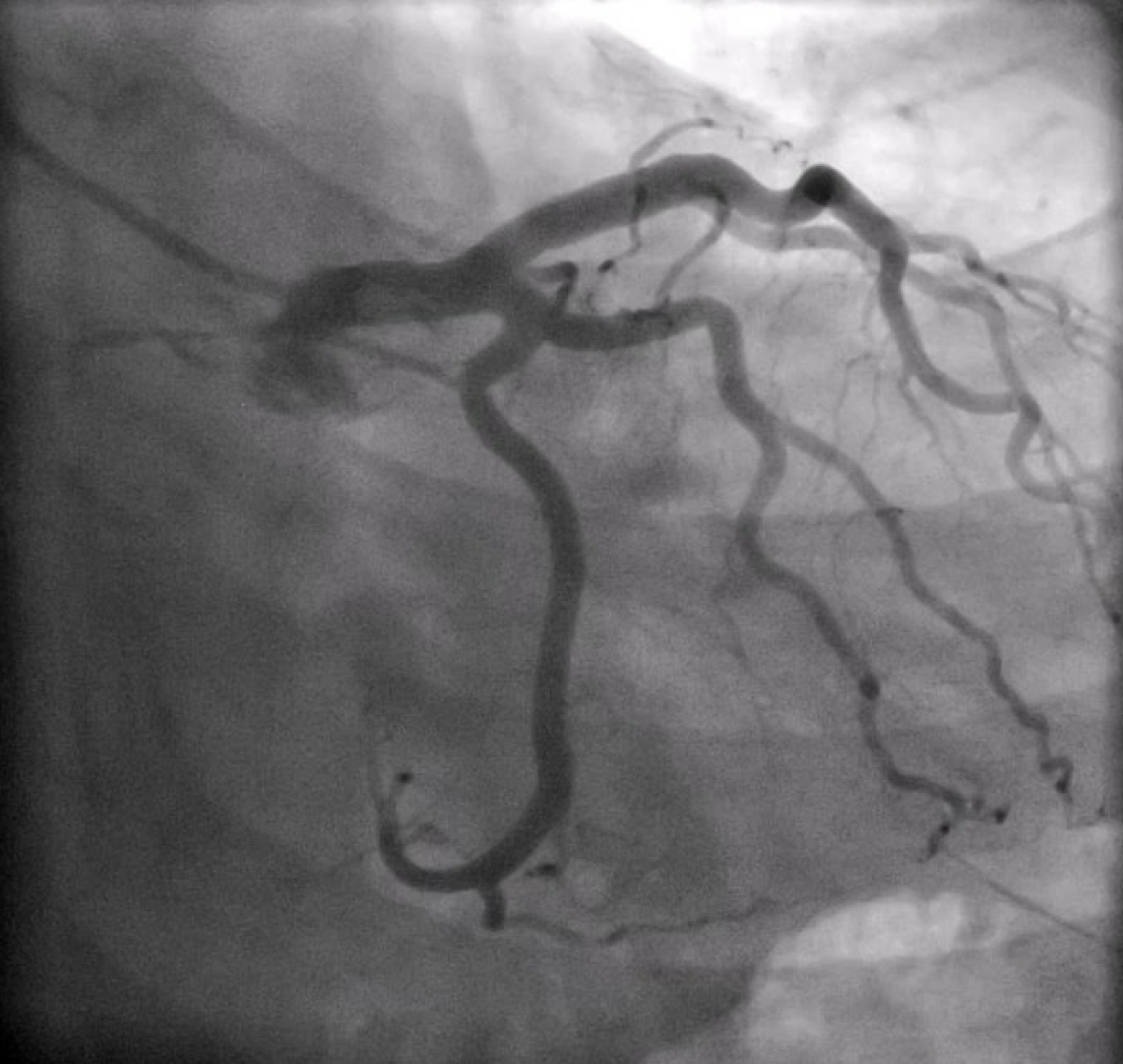
A 36-year-old male with a history of well-controlled HIV on ART, presented with fever, hypotension, and a morbilliform rash shortly after initiation of trimethoprim-sulfamethoxazole for a skin and soft tissue infection. He was found to have elevated troponins (peak 661 ng/L) and diffuse ST elevations on EKG, consistent with myopericarditis. He was vitally stable and did not complain of chest pain or shortness of breath throughout his hospital course. Initial investigation with coronary CTA revealed a possible LM thrombus, which was confirmed on left heart catheterization (LHC) as a non-obstructive thrombus (30% stenosis) in the mid-LM. The patient was managed with a tirofiban bolus and infusion, a heparin drip, and dual antiplatelet therapy with aspirin and clopidogrel. Repeat LHC five days later demonstrated complete resolution of the thrombus. TEE was performed to exclude possible sources of embolization including valvular vegetation or left ventricular thrombus. This was notable for a small mobile echodensity on the tricuspid valve which appeared to be consistent with redundant tissue, but no left-sided source of embolism, and he did not have evidence of a patent foramen ovale. The patient was discharged on apixaban and clopidogrel for 6 and 12 months respectively, with plans for outpatient cardiology follow-up and cardiac MRI.
Conclusion:
In patients with non-obstructive coronary thrombus trigerred by a prothrombotic state, conservative management with anticoagulation and antiplatelet therapy may be appropriate in those who are hemodynamically stable. Clinicians should maintain a high index of suspicion for thrombotic complications in patients with systemic inflammation, especially those with HIV or other prothrombotic risk factors.
Left main (LM) coronary artery thrombus is a rare but life-threatening condition, typically associated with acute coronary syndromes requiring urgent intervention. Certain conditions such as myopericarditis contribute to a prothrombotic state through systemic inflammation. In rare cases, this may predispose to coronary thrombosis, particularly in patients with additional risk factors. We describe a case in which myopericarditis likely contributed to the formation of a non-obstructive left main coronary artery thrombus in the setting of overlapping systemic inflammation and underlying prothrombotic risk, managed conservatively without percutaneous intervention.
Case presentation:
A 36-year-old male with a history of well-controlled HIV on ART, presented with fever, hypotension, and a morbilliform rash shortly after initiation of trimethoprim-sulfamethoxazole for a skin and soft tissue infection. He was found to have elevated troponins (peak 661 ng/L) and diffuse ST elevations on EKG, consistent with myopericarditis. He was vitally stable and did not complain of chest pain or shortness of breath throughout his hospital course. Initial investigation with coronary CTA revealed a possible LM thrombus, which was confirmed on left heart catheterization (LHC) as a non-obstructive thrombus (30% stenosis) in the mid-LM. The patient was managed with a tirofiban bolus and infusion, a heparin drip, and dual antiplatelet therapy with aspirin and clopidogrel. Repeat LHC five days later demonstrated complete resolution of the thrombus. TEE was performed to exclude possible sources of embolization including valvular vegetation or left ventricular thrombus. This was notable for a small mobile echodensity on the tricuspid valve which appeared to be consistent with redundant tissue, but no left-sided source of embolism, and he did not have evidence of a patent foramen ovale. The patient was discharged on apixaban and clopidogrel for 6 and 12 months respectively, with plans for outpatient cardiology follow-up and cardiac MRI.
Conclusion:
In patients with non-obstructive coronary thrombus trigerred by a prothrombotic state, conservative management with anticoagulation and antiplatelet therapy may be appropriate in those who are hemodynamically stable. Clinicians should maintain a high index of suspicion for thrombotic complications in patients with systemic inflammation, especially those with HIV or other prothrombotic risk factors.
More abstracts on this topic:
A Silent Storm: Incidental Discovery of IVC and Right Atrium Thrombus in a Patient with Uterine Stromal Sarcoma
Wasef Natale, Fatima Tehreem, Stys Adam
A Rare Case of Adalimumab-Induced Cardiac Tamponade in a Patient with Psoriatic ArthritisRaval Akhinav, Tran Minh, Saini Ishveen, Rea Mark