Final ID: Su3080
Ischemic ECG Changes Among Patients With Post-PCI Myocardial Injury Are Not Associated With Increased Long-Term All-Cause Mortality
Abstract Body (Do not enter title and authors here): Introduction
Myocardial injury following elective percutaneous coronary intervention (PCI) is associated with reduced long-term survival. Ischemic changes on electrocardiogram (ECG) are an important component of the Universal Definition of Myocardial Infarction (MI), but their prognostic value in the setting of post-PCI myocardial injury remains uncertain.
Research Question
What is the incremental prognostic value of new ischemic ECG changes, or any ischemic ECG findings post-PCI, in patients with post-PCI myocardial injury?
Methods
Adults undergoing elective PCI between 2011 and 2020 without elevated pre-PCI cardiac biomarkers were included if they developed post-PCI myocardial injury, defined by peak CKMB concentration >99% of the upper reference limit. Baseline and post-PCI ECGs (within 24 hours) were reviewed for ischemic ECG findings (ST-segment abnormalities, T-wave abnormalities, and Q-waves), and compared to identify ischemic changes. Long-term mortality was determined from Social Security and National Death Index data. Relationships between ischemic ECG findings and long-term mortality were evaluated in Cox proportional hazards models adjusted for age, sex, and assay-normalized CKMB.
Results
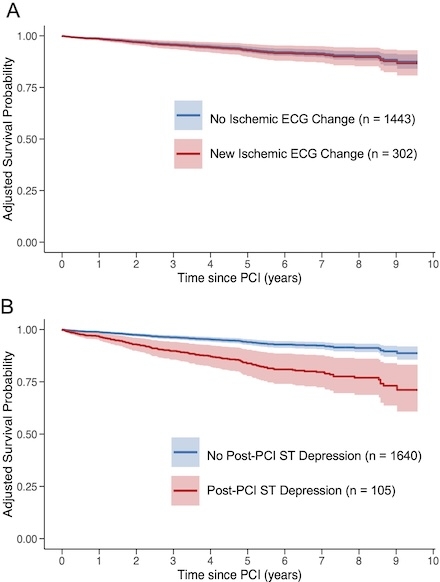
Among 1,745 patients with myocardial injury following elective PCI, 883 (50.6%) had ≥1 ischemic ECG finding post-PCI, and 302 (17.3%) had new ischemic ECG changes from baseline. Median follow-up was 5.2 years with 138 deaths (7.9%). New ischemic ECG changes compared to baseline (n=302) were not associated with increased long-term mortality after multivariable adjustment (7.0% vs. 8.1%, aHR 1.06, 95% CI 0.66–1.71; Figure 1A). When only post-PCI ECGs were considered, the presence of any ischemic finding (n=883) was also not associated with higher mortality (8.5% vs. 7.3%, aHR 1.37, 95% CI 0.98–1.92). In an analysis of ischemic findings on post-PCI ECGs, the presence of any ST-segment depressions (n=105) was associated with increased long-term mortality (16.8% vs. 7.0%, aHR 2.84, 95% CI 1.84–4.38; Figure 1B). Post-PCI ST-segment elevations demonstrated similar but non-significant trends limited by few events.
Conclusion
Among patients with myocardial injury post-PCI, new ischemic ECG changes were not associated with increased mortality. Although the presence of post-PCI ST-segment depressions was associated with increased long-term mortality, other ischemic ECG abnormalities offered limited incremental prognostic value in patients with post-PCI myocardial injury.
Myocardial injury following elective percutaneous coronary intervention (PCI) is associated with reduced long-term survival. Ischemic changes on electrocardiogram (ECG) are an important component of the Universal Definition of Myocardial Infarction (MI), but their prognostic value in the setting of post-PCI myocardial injury remains uncertain.
Research Question
What is the incremental prognostic value of new ischemic ECG changes, or any ischemic ECG findings post-PCI, in patients with post-PCI myocardial injury?
Methods
Adults undergoing elective PCI between 2011 and 2020 without elevated pre-PCI cardiac biomarkers were included if they developed post-PCI myocardial injury, defined by peak CKMB concentration >99% of the upper reference limit. Baseline and post-PCI ECGs (within 24 hours) were reviewed for ischemic ECG findings (ST-segment abnormalities, T-wave abnormalities, and Q-waves), and compared to identify ischemic changes. Long-term mortality was determined from Social Security and National Death Index data. Relationships between ischemic ECG findings and long-term mortality were evaluated in Cox proportional hazards models adjusted for age, sex, and assay-normalized CKMB.
Results
Among 1,745 patients with myocardial injury following elective PCI, 883 (50.6%) had ≥1 ischemic ECG finding post-PCI, and 302 (17.3%) had new ischemic ECG changes from baseline. Median follow-up was 5.2 years with 138 deaths (7.9%). New ischemic ECG changes compared to baseline (n=302) were not associated with increased long-term mortality after multivariable adjustment (7.0% vs. 8.1%, aHR 1.06, 95% CI 0.66–1.71; Figure 1A). When only post-PCI ECGs were considered, the presence of any ischemic finding (n=883) was also not associated with higher mortality (8.5% vs. 7.3%, aHR 1.37, 95% CI 0.98–1.92). In an analysis of ischemic findings on post-PCI ECGs, the presence of any ST-segment depressions (n=105) was associated with increased long-term mortality (16.8% vs. 7.0%, aHR 2.84, 95% CI 1.84–4.38; Figure 1B). Post-PCI ST-segment elevations demonstrated similar but non-significant trends limited by few events.
Conclusion
Among patients with myocardial injury post-PCI, new ischemic ECG changes were not associated with increased mortality. Although the presence of post-PCI ST-segment depressions was associated with increased long-term mortality, other ischemic ECG abnormalities offered limited incremental prognostic value in patients with post-PCI myocardial injury.
More abstracts on this topic:
An individual patient data meta-analysis of complete versus culprit-lesion only revascularization for acute myocardial infarction involving >8,800 individuals: The Complete Revascularization Trialists’ Collaboration
Mehta Shamir, Banning Amerjeet, Ramasundarahettige Chinthanie, Nguyen Helen, Wood David, Engstrom Thomas, Tiong Denise, Böhm Felix, James Stefan, Biscaglia Simone, Campo Gianluca, Smits Pieter, Giacoppo Daniele, Mccann Gerry
Association of Hemoglobin and Partial Pressure of Oxygen in Arterial Blood on Survival and Neurologic Outcomes in In-Hospital Cardiac Arrest PatientsKoul Rudra, Gupta Vasu, Qadeer Nasheeta, Patel Jignesh