Final ID: Su2056
Renal Function, Atrial Cardiopathy, and Their Joint Association with Mortality in the General Population
Abstract Body (Do not enter title and authors here): Background: Growing evidence suggests that left atrial dysfunction, or atrial cardiopathy, significantly increases mortality risk. Similarly, impaired renal function is a well-established predictor of mortality. However, the relationship between impaired renal function and atrial cardiopathy —and how their combined presence affects mortality risk—remains unexplored.
Methods: This analysis included 6,573 participants (mean age 57.0 ± 13.0 years; 50.5% women; 74.6% White) from NHANES-III who underwent electrocardiogram (ECG) recording. We excluded individuals with an estimated glomerular filtration rate (eGFR) <15 mL/min/1.73 m2 or major ECG abnormalities. The CKD-EPI equation was used to calculate eGFR. Atrial cardiopathy was defined from ECG tracings automatically processed at a central core facility as abnormal P-wave axis outside 0–75°, deep terminal negativity in V1 <100 µV, or prolonged P-wave duration in lead II >120 ms. Multivariable logistic regression assessed the cross-sectional association between impaired renal function (eGFR <45 vs. ≥45 mL/min/1.73 m2) and atrial cardiopathy. Cox proportional hazards models evaluated the individual and combined associations of eGFR and atrial cardiopathy with mortality.
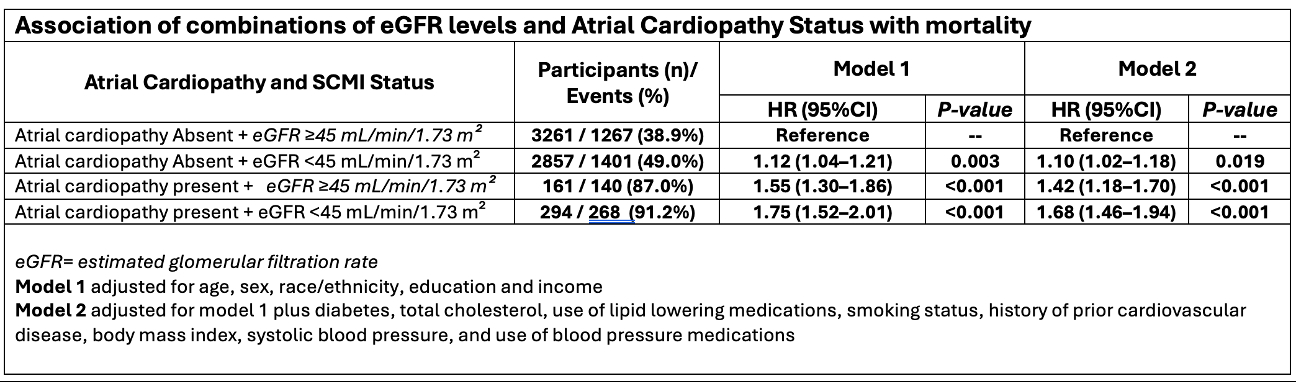
Results: About 47.9% (n=3151) of the participants had atrial cardiopathy at baseline. In multivariable logistic regression model adjusted for sociodemographic and cardiovascular risk factors, eGFR <45 (compared to ≥45) mL/min/1.73 m2 was associated with increased risk of atrial cardiopathy (OR (95% CI): 1.44(1.16–1.78)). During a median follow-up of 18.1 years, 3076 deaths occurred. Separate multivariable Cox proportional hazards models demonstrated that both atrial cardiopathy and eGFR <45 mL/min/1.73 m2 (compared to ≥45) were associated with an increased risk of mortality (HR (95% CI): 1.12(1.04-1.20) and 1.50(1.34-1.68), respectively). Compared to participants with eGFR ≥ 45 mL/min/1.73 m2 without atrial cardiopathy CM (reference group), those with coexistent eGFR <45 mL/min/1.73 m2 and atrial cardiopathy exhibited substantially higher risk of mortality, which was higher than either condition alone; interaction p-value = 0.011(Table).
Conclusions: Impaired renal function is associated with increased risk of atrial cardiopathy, and both conditions independently predict mortality, and their coexistence exhibits a synergistic effect, substantially amplifying mortality risk beyond their individual contributions.
Methods: This analysis included 6,573 participants (mean age 57.0 ± 13.0 years; 50.5% women; 74.6% White) from NHANES-III who underwent electrocardiogram (ECG) recording. We excluded individuals with an estimated glomerular filtration rate (eGFR) <15 mL/min/1.73 m2 or major ECG abnormalities. The CKD-EPI equation was used to calculate eGFR. Atrial cardiopathy was defined from ECG tracings automatically processed at a central core facility as abnormal P-wave axis outside 0–75°, deep terminal negativity in V1 <100 µV, or prolonged P-wave duration in lead II >120 ms. Multivariable logistic regression assessed the cross-sectional association between impaired renal function (eGFR <45 vs. ≥45 mL/min/1.73 m2) and atrial cardiopathy. Cox proportional hazards models evaluated the individual and combined associations of eGFR and atrial cardiopathy with mortality.
Results: About 47.9% (n=3151) of the participants had atrial cardiopathy at baseline. In multivariable logistic regression model adjusted for sociodemographic and cardiovascular risk factors, eGFR <45 (compared to ≥45) mL/min/1.73 m2 was associated with increased risk of atrial cardiopathy (OR (95% CI): 1.44(1.16–1.78)). During a median follow-up of 18.1 years, 3076 deaths occurred. Separate multivariable Cox proportional hazards models demonstrated that both atrial cardiopathy and eGFR <45 mL/min/1.73 m2 (compared to ≥45) were associated with an increased risk of mortality (HR (95% CI): 1.12(1.04-1.20) and 1.50(1.34-1.68), respectively). Compared to participants with eGFR ≥ 45 mL/min/1.73 m2 without atrial cardiopathy CM (reference group), those with coexistent eGFR <45 mL/min/1.73 m2 and atrial cardiopathy exhibited substantially higher risk of mortality, which was higher than either condition alone; interaction p-value = 0.011(Table).
Conclusions: Impaired renal function is associated with increased risk of atrial cardiopathy, and both conditions independently predict mortality, and their coexistence exhibits a synergistic effect, substantially amplifying mortality risk beyond their individual contributions.
More abstracts on this topic:
Association between Alcohol Consumption and the Risk of Cardiovascular Events by Renal Function Status in Japanese Community Dwellers
Hirata Aya, Sugiyama Daisuke, Okamura Tomonori, Takebayashi Toru, Harada Sei, Iida Miho, Miyagawa Naoko, Matsumoto Minako, Shibuki Takuma, Toki Ryota, Edagawa Shun, Kuwabara Kazuyo
Causal Association of Left Atrial Emptying Fraction With Ischemic Stroke: A Mendelian Randomization AnalysisNguyen Kevin, Cole John, Perry James, Gaynor Brady, Bai Zilong, Wang Fei, Xu Huichun, Leifer Dana