Final ID: MP312
Total Carotid Artery Calcium Score on Standard-of-care Oncologic Computed Tomography Scans Predicts Radiation-induced Carotid Artery Disease and its Sequelae in Patients with Oropharyngeal Cancer
Methods:Patients with OPC treated with RT at a tertiary center during 2016-19 were identified. SOC oncologic pre-RT CT of the neck with contrast was used to estimate CaACS utilizing the CT Cardiac package of SyngoVia (Siemens Healthcare). To separate calcified plaque from contrast, density threshold of 230 HU was used.Bilateral common and internal carotid arteries were evaluated to the C1 vertebra. Patients were split into three groups based on CaACS distribution:low (values ≤ median) as reference group,medium(values between median and 75th percentile),and high (values >75th percentile).
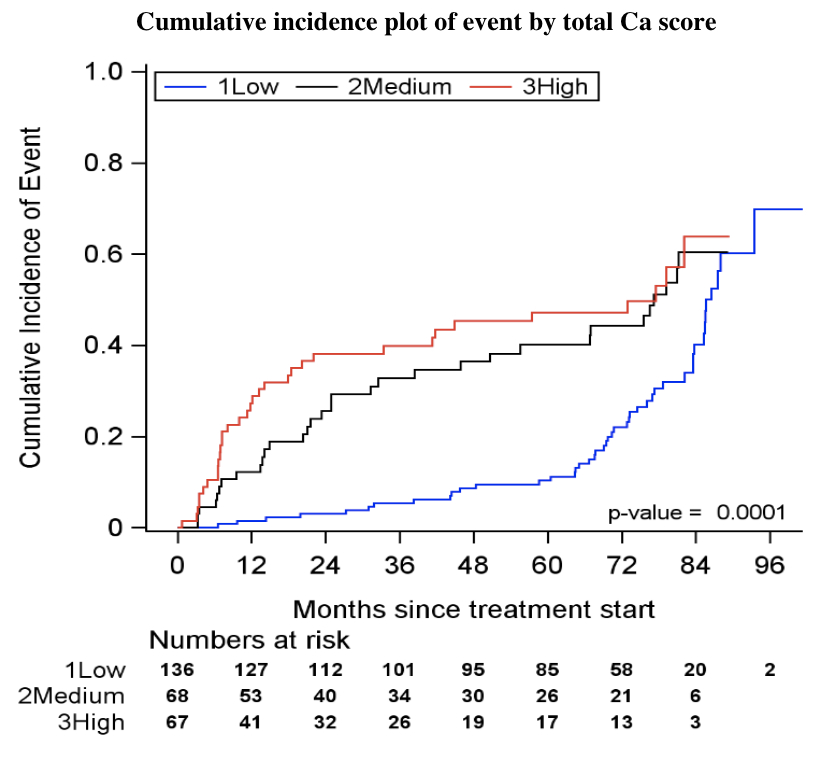
Results:A total of 271 patients were included (mean age 61 ± 9.8, 88% male).Smoking was reported in 57%, hypertension (HTN) in 53%, dyslipidemia (DLD) in 43%, and diabetes mellitus (DM) in 14%,while 34% were on a statin prior to RT. Total median CaACS was 10.8 AU (IQR 0-140.6) with 46% having a score of 0. During a median follow up of 6.4 years (IQR 6.3-6.6), 41% developed new or worsened carotid atherosclerosis, 3.7% carotid artery stenosis >50%, 2.6% TIA or stroke, and 17% died without new or worsened carotid atherosclerosis. In a multivariate cause-specific Cox regression analysis, high CaACS was significantly associated with increased risk of the composite outcome of worsened carotid atherosclerosis, >50% stenosis, TIA or stroke (HR 2.18,95% CI[1.34-3.54]) compared to low CaACS. Hypertension was also associated with the composite outcome (2.26[1.49-3.41]) while no significant associations were noted with age, smoking, DLD, DM, or statin use. Fine-Gray analysis showed similar results.
Conclusion:In our cohort of patients with OPC, high CaACS and history of HTN prior to RT, were significantly associated with development of RICAD. Quantification of carotid artery calcific atherosclerosis utilizing SOC oncologic CT imaging may assist with patient risk stratification, guide surveillance and potentially mitigate RICAD in OPC survivors.
- Kapadia, Taher ( MD Anderson Cancer Center , Houston , Texas , United States )
- Lin, Ruitao ( MD Anderson Cancer Center , Houston , Texas , United States )
- Abe, Junichi ( University of Texas MD Anderson Can , Houston , Texas , United States )
- Palaskas, Nicolas ( UT MD Anderson Cancer Center , Houston , Texas , United States )
- Gladish, Gregory ( MD Anderson Cancer Center , Houston , Texas , United States )
- Moreno, Amy ( MD Anderson Cancer Center , Houston , Texas , United States )
- Naser, Mohamed ( MD Anderson Cancer Center , Houston , Texas , United States )
- Hutcheson, Katherine ( MD Anderson Cancer Center , Houston , Texas , United States )
- Rosenthal, David ( MD Anderson Cancer Center , Houston , Texas , United States )
- Mouhayar, Elie ( MD Anderson Cancer Center , Houston , Texas , United States )
- Deswal, Anita ( UT MD Anderson Cancer Center , Houston , Texas , United States )
- Bandrey, Dhawal Sanjay ( MD Anderson Cancer Center , Houston , Texas , United States )
- Fuller, Clifton ( MD Anderson Cancer Center , Houston , Texas , United States )
- Viguet, Claire ( Mcgovern Medical School , Houston , Texas , United States )
- Koutroumpakis, Efstratios ( MD Anderson Cancer Center , Houston , Texas , United States )
- Patel, Bhumiben ( MD Anderson Cancer Center , Houston , Texas , United States )
- Van Bergen Diaz, Patrik Joan ( University of Barcelona , Barcelona , Spain )
- Shen, Jennifer ( MD Anderson Cancer Center , Pearland , Texas , United States )
- Mbagwu, Gabrielle ( MD Anderson Cancer Center , Houston , Texas , United States )
- Patin, Stephen ( MD Anderson Cancer Center , Houston , Texas , United States )
- Hughes, Andres ( MD Anderson Cancer Center , Houston , Texas , United States )
- Song, Juhee ( MD Anderson Cancer Center , Houston , Texas , United States )
Meeting Info:
Session Info:
Cardiac Imaging in Cancer Therapy: Risk Prediction, Detection, and AI-Driven Insight
Saturday, 11/08/2025 , 12:15PM - 01:25PM
Moderated Digital Poster Session
More abstracts on this topic:
Jackson William, Zhu Ashley, Gu Wenduo, Berezowitz Alexa, Iyer Meghana, Cheng Paul
A Cardiac Ryanodine Receptor C-terminal Truncation Causes Calcium Release Deficiency Syndrome, but not Catecholaminergic Polymorphic Ventricular TachycardiaTian Shanshan, Ni Mingke, Wang Hui, Zhu Hai-lei, Wang Ruiwu, Estillore John Paul, Chen Wayne
More abstracts from these authors:
Bandrey Dhawal Sanjay, Abe Junichi, Lin Ruitao, Moreno Amy, Naser Mohamed, Hutcheson Kate, Rosenthal David, Khalaf Shaden, Iliescu Cezar, Mouhayar Elie, Deswal Anita, Patel Bhumiben, Fuller Clifton, Koutroumpakis Efstratios, Van Bergen Diaz Patrik Joan, Mbagwu Gabrielle, Shen Jennifer, Kapadia Taher, Patin Stephen, Hughes Andres, Song Juhee
Longitudinal Echocardiographic Assessment of Subacute Cardiotoxicity in a Prospective Cohort of Adolescents and Young Adults with Sarcoma Treated with High-Dose DoxorubicinViguet Claire, Chandra Joya, Daw Najat, Hildebrandt Michelle, Livingston John, Ali Hj, Roth Michael, Kleinerman Eugenie, Deswal Anita, Koutroumpakis Efstratios, Hughes Andres, Banchs Jose, Kapadia Taher, Gilchrist Susan, Rauschendorfer Savannah, Jeyabal Prince, Song Juhee, Honey Theresa