Final ID: MP2567
Neck Adiposity Measured on Pre-therapy Oncologic Computed Tomography Scans Predicts the Development of Radiation Therapy-induced Carotid Artery Disease in Patients with Head and Neck Cancer
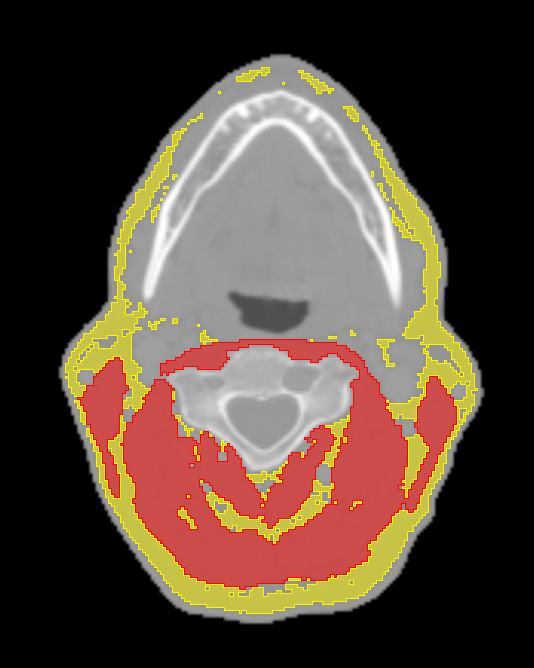
Methods Patients with HNC treated with RT at a tertiary center between 2005 and 2010 were identified. Oncologic CT scans of the neck performed for RT planning purposes were used to quantify adipose tissue and skeletal muscle mass at the C3 spinal level by SliceOmatic, version 5.0 Tomovision (Figure 1). Adipose tissue and skeletal muscle volumes were indexed to account for height. Fine-Gray competing risk regression models with stepwise forward selection were used to evaluate the association between baseline clinical and imaging characteristics with subsequent development of the composite event of new or worsened carotid atherosclerosis, carotid artery stenosis >50%, transient ischemic attack (TIA) or stroke.
Results Of 231 patients, 91% were male and 97% white, with a mean age of 74 ± 9 years. Prior to RT, 42% had hypertension, 28% dyslipidemia, 12% diabetes, and 3.5% prior stroke/TIA. At a median follow-up of 9.8 years (IQR 10.5), 42% developed new or worsened carotid atherosclerosis, 12% carotid stenosis >50%, and 6% stroke/TIA, while 39% expired. In the multivariable Fine-Gray analysis, neck adipose tissue index was significantly associated with the development of the composite event (HR 1.04 per unit increase, 95% CI 1.01–1.06, p = 0.0015). Baseline use of antiplatelet agents was also associated with the composite event (HR 2.18, 95% CI 1.41–3.36, p = 0.0004) while no significant association was noted with other characteristics such as age, traditional cardiovascular risk factors, prior atherosclerotic disease, statin use, RT dose and skeletal muscle mass.
Conclusion Neck adiposity was associated with RICAD in our cohort of HNC patients with long follow up, supporting the hypothesis of an interplay between inflamed perivascular adiposity and development of carotid artery disease post RT in survivors of HNC. Adipose tissue quantification using SOC oncologic CT scans may assist with patient risk stratification and guide surveillance.
- Bandrey, Dhawal Sanjay ( UT MD Anderson Cancer Center , Houston , Texas , United States )
- Abe, Junichi ( UT MD Anderson Cancer Center , Houston , Texas , United States )
- Lin, Ruitao ( UT MD Anderson Cancer Center , Houston , Texas , United States )
- Moreno, Amy ( UT MD Anderson Cancer Center , Houston , Texas , United States )
- Naser, Mohamed ( UT MD Anderson Cancer Center , Houston , Texas , United States )
- Hutcheson, Kate ( UT MD Anderson Cancer Center , Houston , Texas , United States )
- Rosenthal, David ( UT MD Anderson Cancer Center , Houston , Texas , United States )
- Khalaf, Shaden ( UT MD Anderson Cancer Center , Houston , Texas , United States )
- Iliescu, Cezar ( UT MD Anderson Cancer Center , Houston , Texas , United States )
- Mouhayar, Elie ( UT MD Anderson Cancer Center , Houston , Texas , United States )
- Deswal, Anita ( UT MD Anderson Cancer Center , Houston , Texas , United States )
- Patel, Bhumiben ( UT MD Anderson Cancer Center , Houston , Texas , United States )
- Fuller, Clifton ( UT MD Anderson Cancer Center , Houston , Texas , United States )
- Koutroumpakis, Efstratios ( UT MD Anderson Cancer Center , Houston , Texas , United States )
- Van Bergen Diaz, Patrik Joan ( University of Barcelona , Barcelona , Spain )
- Mbagwu, Gabrielle ( UT MD Anderson Cancer Center , Houston , Texas , United States )
- Shen, Jennifer ( UT MD Anderson Cancer Center , Houston , Texas , United States )
- Kapadia, Taher ( UT MD Anderson Cancer Center , Houston , Texas , United States )
- Patin, Stephen ( UT MD Anderson Cancer Center , Houston , Texas , United States )
- Hughes, Andres ( UT MD Anderson Cancer Center , Houston , Texas , United States )
- Song, Juhee ( UT MD Anderson Cancer Center , Houston , Texas , United States )
Meeting Info:
Session Info:
More abstracts on this topic:
Chirivi Miguel, Rendon Javier, Lauver Adam, Fink Gregory, Watts Stephanie, Contreras Andres
Adipose tissue extracellular vesicles mediate pro-arrhythmic changes in atrial cardiomyocytesLimpitikul Worawan, Garcia Contreras Marta, Betti Michael, Sheng Quanhu, Xiao Ling, Chatterjee Emeli, Gamazon Eric, Shah Ravi, Das Saumya
More abstracts from these authors:
Wang Emily, Palaskas Nicolas, Ali Hyeon-ju, Ostos Mendoza Keila, Koutroumpakis Efstratios, Khalaf Shaden, Hamzeh Ihab, Kumar Salil, Iliescu Cezar, Deswal Anita
Total Carotid Artery Calcium Score on Standard-of-care Oncologic Computed Tomography Scans Predicts Radiation-induced Carotid Artery Disease and its Sequelae in Patients with Oropharyngeal CancerKapadia Taher, Lin Ruitao, Abe Junichi, Palaskas Nicolas, Gladish Gregory, Moreno Amy, Naser Mohamed, Hutcheson Katherine, Rosenthal David, Mouhayar Elie, Deswal Anita, Bandrey Dhawal Sanjay, Fuller Clifton, Viguet Claire, Koutroumpakis Efstratios, Patel Bhumiben, Van Bergen Diaz Patrik Joan, Shen Jennifer, Mbagwu Gabrielle, Patin Stephen, Hughes Andres, Song Juhee