Final ID: MP1228
ECMO Combined with Thrombectomy Yields Superior Outcomes in Acute High-Risk Pulmonary Embolism
Abstract Body (Do not enter title and authors here): Background:
Extracorporeal membrane oxygenation (ECMO) is used as a rescue therapy in patients with severe high-risk pulmonary embolism (PE), but data on optimal management and especially on mid- and long-term outcomes remain limited.
Hypothesis:
We hypothesized that ECMO combined with thrombectomy would lead to better short- and long-term outcomes than ECMO with thrombolysis or ECMO alone.
Methods:
We retrospectively reviewed the medical records of patients with high-risk PE who received ECMO at a single institution between January 2016 and July 2024. Patients were categorized into three groups based on the type of adjunctive reperfusion therapy received: those who underwent thrombectomy, including surgical and percutaneous mechanical thrombectomy; those who received thrombolysis, including systemic thrombolysis and catheter-directed thrombolysis; and those who were managed with ECMO alone without reperfusion therapy. We compared patient characteristics and clinical outcomes across these groups.
Results:
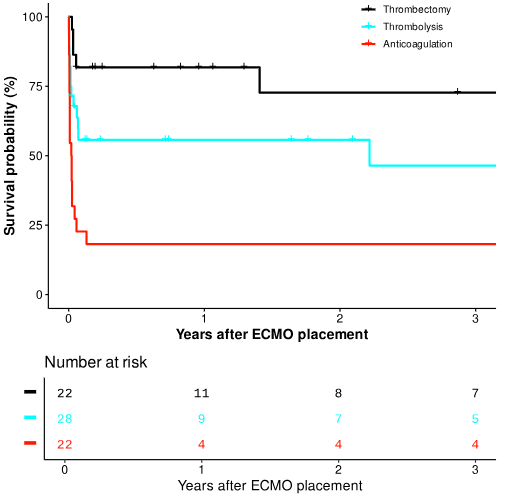
A total of 72 patients with high-risk PE underwent ECMO during the study period, with a median age of 52.5 years (95% CI: 42.0–65.3). Of these, 22 patients received ECMO with thrombectomy (5 surgical, 17 percutaneous), 28 patients received ECMO with thrombolysis (13 systemic, 15 catheter-directed), and 22 patients received ECMO alone. There were no significant demographic differences among the groups. The incidence of cardiac arrest was similar: ECMO alone (72.7%), thrombolysis (67.9%), and thrombectomy (77.3%) (P=0.76). The median duration of ECMO support was 5 days (95% CI: 4–6 days), with no significant difference among the three groups (P = 0.2). Successful weaning from ECMO was achieved in 100% of the thrombectomy group, 60.7% of the thrombolysis group, and 36.4% of the ECMO-alone group (P<0.01). Survival to hospital discharge was highest in the ECMO with thrombectomy group (81.8%), compared to 57.1% in the thrombolysis group and 18.1% in the ECMO alone group (P<0.01). There were no significant differences in in-hospital complications among the groups. The 1- and 3-year survival rates were 81.8%, and 72.7% in the ECMO with thrombectomy group; 55.7%, and 46.4% in the ECMO with thrombolysis group; and 18.2%, and 18.2% in the ECMO alone group (P <0.001).
Conclusion:
ECMO without reperfusion therapy was associated with poor outcomes, whereas ECMO with thrombectomy provided the best short- and long-term survival, followed by thrombolysis.
Extracorporeal membrane oxygenation (ECMO) is used as a rescue therapy in patients with severe high-risk pulmonary embolism (PE), but data on optimal management and especially on mid- and long-term outcomes remain limited.
Hypothesis:
We hypothesized that ECMO combined with thrombectomy would lead to better short- and long-term outcomes than ECMO with thrombolysis or ECMO alone.
Methods:
We retrospectively reviewed the medical records of patients with high-risk PE who received ECMO at a single institution between January 2016 and July 2024. Patients were categorized into three groups based on the type of adjunctive reperfusion therapy received: those who underwent thrombectomy, including surgical and percutaneous mechanical thrombectomy; those who received thrombolysis, including systemic thrombolysis and catheter-directed thrombolysis; and those who were managed with ECMO alone without reperfusion therapy. We compared patient characteristics and clinical outcomes across these groups.
Results:
A total of 72 patients with high-risk PE underwent ECMO during the study period, with a median age of 52.5 years (95% CI: 42.0–65.3). Of these, 22 patients received ECMO with thrombectomy (5 surgical, 17 percutaneous), 28 patients received ECMO with thrombolysis (13 systemic, 15 catheter-directed), and 22 patients received ECMO alone. There were no significant demographic differences among the groups. The incidence of cardiac arrest was similar: ECMO alone (72.7%), thrombolysis (67.9%), and thrombectomy (77.3%) (P=0.76). The median duration of ECMO support was 5 days (95% CI: 4–6 days), with no significant difference among the three groups (P = 0.2). Successful weaning from ECMO was achieved in 100% of the thrombectomy group, 60.7% of the thrombolysis group, and 36.4% of the ECMO-alone group (P<0.01). Survival to hospital discharge was highest in the ECMO with thrombectomy group (81.8%), compared to 57.1% in the thrombolysis group and 18.1% in the ECMO alone group (P<0.01). There were no significant differences in in-hospital complications among the groups. The 1- and 3-year survival rates were 81.8%, and 72.7% in the ECMO with thrombectomy group; 55.7%, and 46.4% in the ECMO with thrombolysis group; and 18.2%, and 18.2% in the ECMO alone group (P <0.001).
Conclusion:
ECMO without reperfusion therapy was associated with poor outcomes, whereas ECMO with thrombectomy provided the best short- and long-term survival, followed by thrombolysis.
More abstracts on this topic:
Catheter-Directed Intervention for High-Risk Acute Pulmonary Embolism in Chronic Kidney Disease
Kumar Manoj, Ricciardi Mark, Arman Qamar, Ali Shafaqat, Jamshed Aneeza, Murthi Mukunthan, Kumar Nomesh, Kumar Sanjay, Kumari Rinkle, Alraies M Chadi, Gomez Valencia Javier
Brain-Directed Management of Venoarterial Extracorporeal Membrane Oxygenation in a Pediatric Swine ModelKo Tiffany, Seeney Alyssa, Krishna Akshatha, Goto Rika, Lewis Alistair, Hurlock April, Lin Yuxi, Hwang Misun, Senthil Kumaran, Aronowitz Danielle, Spelde Audrey, Terakawa Katsunari, Morgan Ryan, Mavroudis Constantine, Baker Wesley, Kilbaugh Todd, Smood Benjamin, Slovis Julia, Menezes Forti Rodrigo, Melchior Richard, Sueishi Takayuki, Chalifoux Nolan, Ranieri Nicolina