Final ID: MP78
A Perfect Storm: Simultaneous Pulmonary Embolism, STEMI, and Stroke via Paradoxical Embolism in a Hospitalized Patient on DVT Prophylaxis
Abstract Body (Do not enter title and authors here): Background
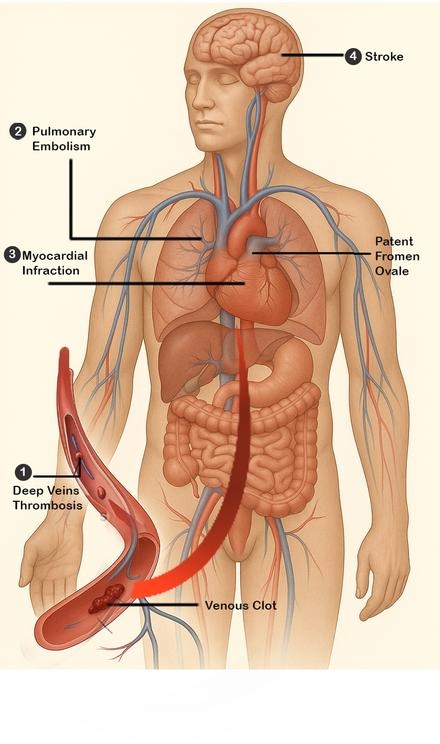
Simultaneous cardio-cerebral embolism is rare, and its co-occurrence with pulmonary embolism (PE) is exceedingly uncommon. This triad often results from paradoxical embolism through a patent foramen ovale (PFO), especially under acute right heart strain. Such cases pose significant diagnostic and therapeutic challenges requiring rapid, multidisciplinary coordination.
Case
A 70-year-old woman with prior cervical cancer (post-hysterectomy) and remote provoked DVT presented with nausea, vomiting, weakness, and small bowel obstruction (SBO), confirmed on CT. She was treated conservatively with NG decompression and subcutaneous heparin for DVT prophylaxis. On hospital day 4, she developed sudden neurological deficits and chest pain. ECG showed STEMI with heart block. CT angiography revealed bilateral PE and a right MCA infarct. She developed pulseless electrical activity (PEA) during imaging and achieved return of spontaneous circulation (ROSC) after CPR. A second cardiac arrest in the ICU also resulted in ROSC.
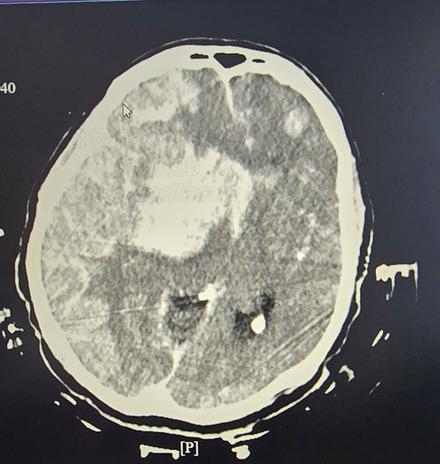
She received systemic tPA for both PE and stroke, underwent RCA thrombectomy, and had a temporary pacemaker placed. Planned mechanical thrombectomy was aborted after imaging showed haemorrhagic infarction, cerebral edema, and herniation. Echocardiography revealed a PFO, suggesting paradoxical embolism. Despite aggressive ICU management, her neurological condition deteriorated, and following confirmation of brain death, care was transitioned to comfort measures.
Discussion
This case illustrates the complexity of managing simultaneous PE, STEMI, and stroke. Despite ambulation and prophylaxis, the patient developed catastrophic embolic events likely due to paradoxical embolism across a PFO triggered by sub massive PE. The thrombus source remains uncertain, ranging from undetected DVT to mesenteric thrombosis or evolving hypercoagulability. Systemic thrombolysis was used for a broad effect but led to haemorrhagic transformation, a known risk in large infarcts.
Conclusion
This case highlights the importance of early recognition and multidisciplinary management of rare multisystem embolic events. It also underscores the limitations of routine prophylaxis in high-risk inpatients. In the absence of established protocols, individualized care and further research are essential. This report contributes to the limited literature on this triad and reinforces paradoxical embolism as a unifying mechanism.
Simultaneous cardio-cerebral embolism is rare, and its co-occurrence with pulmonary embolism (PE) is exceedingly uncommon. This triad often results from paradoxical embolism through a patent foramen ovale (PFO), especially under acute right heart strain. Such cases pose significant diagnostic and therapeutic challenges requiring rapid, multidisciplinary coordination.
Case
A 70-year-old woman with prior cervical cancer (post-hysterectomy) and remote provoked DVT presented with nausea, vomiting, weakness, and small bowel obstruction (SBO), confirmed on CT. She was treated conservatively with NG decompression and subcutaneous heparin for DVT prophylaxis. On hospital day 4, she developed sudden neurological deficits and chest pain. ECG showed STEMI with heart block. CT angiography revealed bilateral PE and a right MCA infarct. She developed pulseless electrical activity (PEA) during imaging and achieved return of spontaneous circulation (ROSC) after CPR. A second cardiac arrest in the ICU also resulted in ROSC.
She received systemic tPA for both PE and stroke, underwent RCA thrombectomy, and had a temporary pacemaker placed. Planned mechanical thrombectomy was aborted after imaging showed haemorrhagic infarction, cerebral edema, and herniation. Echocardiography revealed a PFO, suggesting paradoxical embolism. Despite aggressive ICU management, her neurological condition deteriorated, and following confirmation of brain death, care was transitioned to comfort measures.
Discussion
This case illustrates the complexity of managing simultaneous PE, STEMI, and stroke. Despite ambulation and prophylaxis, the patient developed catastrophic embolic events likely due to paradoxical embolism across a PFO triggered by sub massive PE. The thrombus source remains uncertain, ranging from undetected DVT to mesenteric thrombosis or evolving hypercoagulability. Systemic thrombolysis was used for a broad effect but led to haemorrhagic transformation, a known risk in large infarcts.
Conclusion
This case highlights the importance of early recognition and multidisciplinary management of rare multisystem embolic events. It also underscores the limitations of routine prophylaxis in high-risk inpatients. In the absence of established protocols, individualized care and further research are essential. This report contributes to the limited literature on this triad and reinforces paradoxical embolism as a unifying mechanism.
More abstracts on this topic:
Heart of the Mystery: Unveiling PFO's Role in Cryptogenic Stroke During Pregnancy
Bagha Zohaib, Ali Zohair, Wilson Sean, Grayver Evelina
A Contactless and Automated Approach to the Acute Stroke AssessmentSaadat Moh, Titus Ryan, Verkuilen Haley, Fleming Phil, Sur Sanjib, Sen Souvik