Final ID: Mo2095
Self-Reported Loneliness Independently Predicts Cardiovascular Mortality in a Diverse National Cohort
Abstract Body (Do not enter title and authors here): Background: Loneliness is a growing public health concern. In 2022, the AHA identified it as a contributor to poor cardiovascular health, followed by a 2023 U.S. Surgeon General advisory declaring an “Epidemic of Loneliness and Isolation”. Although linked to mortality, its independent effect and generalizability across diverse groups remain understudied. With over half of U.S. adults reporting loneliness, understanding its role may be essential to improving cardiovascular outcomes.
Research Questions/Hypothesis: We examined the association between loneliness and CVD mortality in a diverse national cohort. We hypothesized that loneliness would be associated with increased CVD mortality.
Methods: The Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study is a prospective cohort of 30,239 adults aged ≥45 years recruited from 2003-2007. We included those who completed a baseline loneliness item assessing feelings in the past week. Cox proportional hazards models estimated HRs and 95% CIs for the association between loneliness and time to CVD death. Models were sequentially adjusted for demographics (age, race, gender), SDOH (employment, education, income, insurance, region, poverty, health professional shortage, public health infrastructure), clinical factors (hypertension, diabetes, self-rated physical health, obesity, inflammation, cognition), health behaviors (smoking, activity, diet, medication adherence), and objective social health (partnership, social isolation, social support). Effect modification by age, race, and gender was assessed using interaction terms.
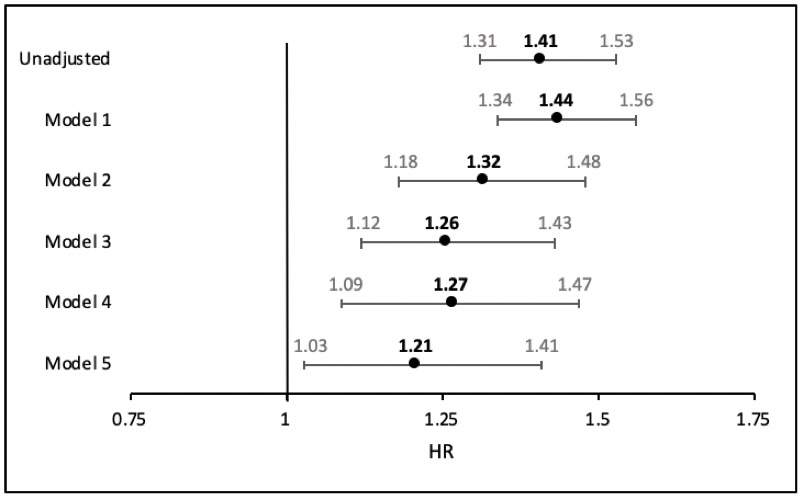
Results: We included 29,387 participants with median follow-up of 13.1 years (IQR 7.3-16.1). Mean age was 65.0 years (SD 9.4); 41% identified as Non-Hispanic Black and 55% were women. Overall, 21% of participants reported loneliness in the past week, with 3,643 CVD deaths observed. Loneliness was associated with a 41% increased hazard of CVD mortality in unadjusted models (HR, 1.41; 95% CI, 1.31-1.53). The association attenuated but remained significant in the fully adjusted model (HR, 1.21; 95% CI, 1.03-1.41). No effect modification was observed.
Conclusion: Loneliness was associated with increased CVD mortality risk, even after accounting for clinical, behavioral, and social factors. A one-time, self-reported loneliness measure may serve as a practical tool for identifying at-risk patients and inform efforts to reduce cardiovascular risk.
Research Questions/Hypothesis: We examined the association between loneliness and CVD mortality in a diverse national cohort. We hypothesized that loneliness would be associated with increased CVD mortality.
Methods: The Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study is a prospective cohort of 30,239 adults aged ≥45 years recruited from 2003-2007. We included those who completed a baseline loneliness item assessing feelings in the past week. Cox proportional hazards models estimated HRs and 95% CIs for the association between loneliness and time to CVD death. Models were sequentially adjusted for demographics (age, race, gender), SDOH (employment, education, income, insurance, region, poverty, health professional shortage, public health infrastructure), clinical factors (hypertension, diabetes, self-rated physical health, obesity, inflammation, cognition), health behaviors (smoking, activity, diet, medication adherence), and objective social health (partnership, social isolation, social support). Effect modification by age, race, and gender was assessed using interaction terms.
Results: We included 29,387 participants with median follow-up of 13.1 years (IQR 7.3-16.1). Mean age was 65.0 years (SD 9.4); 41% identified as Non-Hispanic Black and 55% were women. Overall, 21% of participants reported loneliness in the past week, with 3,643 CVD deaths observed. Loneliness was associated with a 41% increased hazard of CVD mortality in unadjusted models (HR, 1.41; 95% CI, 1.31-1.53). The association attenuated but remained significant in the fully adjusted model (HR, 1.21; 95% CI, 1.03-1.41). No effect modification was observed.
Conclusion: Loneliness was associated with increased CVD mortality risk, even after accounting for clinical, behavioral, and social factors. A one-time, self-reported loneliness measure may serve as a practical tool for identifying at-risk patients and inform efforts to reduce cardiovascular risk.
More abstracts on this topic:
A Meta-Analysis on the Effect of Chronic Total Occlusion of Coronary Arteries on Cardiovascular Outcomes in Patients Undergoing Transcatheter Aortic Valve Replacement
Goyal Aman, Tariq Muhammad Daoud, Zahra Rubab, Jain Hritvik, Khan Rozi, Mahalwar Gauranga
A New Biomarker of Aging Derived From Electrocardiogram Improves Risk Prediction of Incident Myocardial Infarction and Stroke.Wilsgaard Tom, Rosamond Wayne, Schirmer Henrik, Lindekleiv Haakon, Attia Zachi, Lopez-jimenez Francisco, Leon David, Iakunchykova Olena