Final ID: MP2366
Closing Prevention Gaps in Women’s Heart Health: Real-World Impact of a Scalable Group Virtual Care Model
Abstract Body (Do not enter title and authors here):
Introduction: Cardiovascular disease (CVD) is the leading cause of death for women in the United States, yet prevention gaps persist due to provider shortages, underrecognition of sex-specific risk factors, and declining public and professional awareness of the burden of CVD in women. Scalable models that address workforce constraints and enable timely, preventive care for women—such as virtual shared medical appointments—remain poorly defined.
Objective: To evaluate the impact of a virtual shared medical appointment (SMA) model on CV risk factor optimization in women with elevated cardiometabolic risk and/or established CVD.
Methods: Systole Health, a group virtual care organization, enrolled 13 cohorts of 3–5 women into a six-week CV prevention program across 16 U.S. states (April 2024–May 2025). Eligible participants had documented or self-reported overweight/obesity, hypertension (HTN), dyslipidemia (DLD), (pre)diabetes, and/or established CVD. Exclusion criteria included active pregnancy and unstable CVD. The intervention included weekly physician-led SMAs, lifestyle health coaching, and peer support. Medication management was offered to a subset of patients based on clinical need. Outcomes were assessed at baseline and program completion, including self-reported body mass index (BMI), blood pressure (BP) (average of one week of home readings), and LDL cholesterol (LDL-C). Paired two-sample t-tests assessed mean changes.
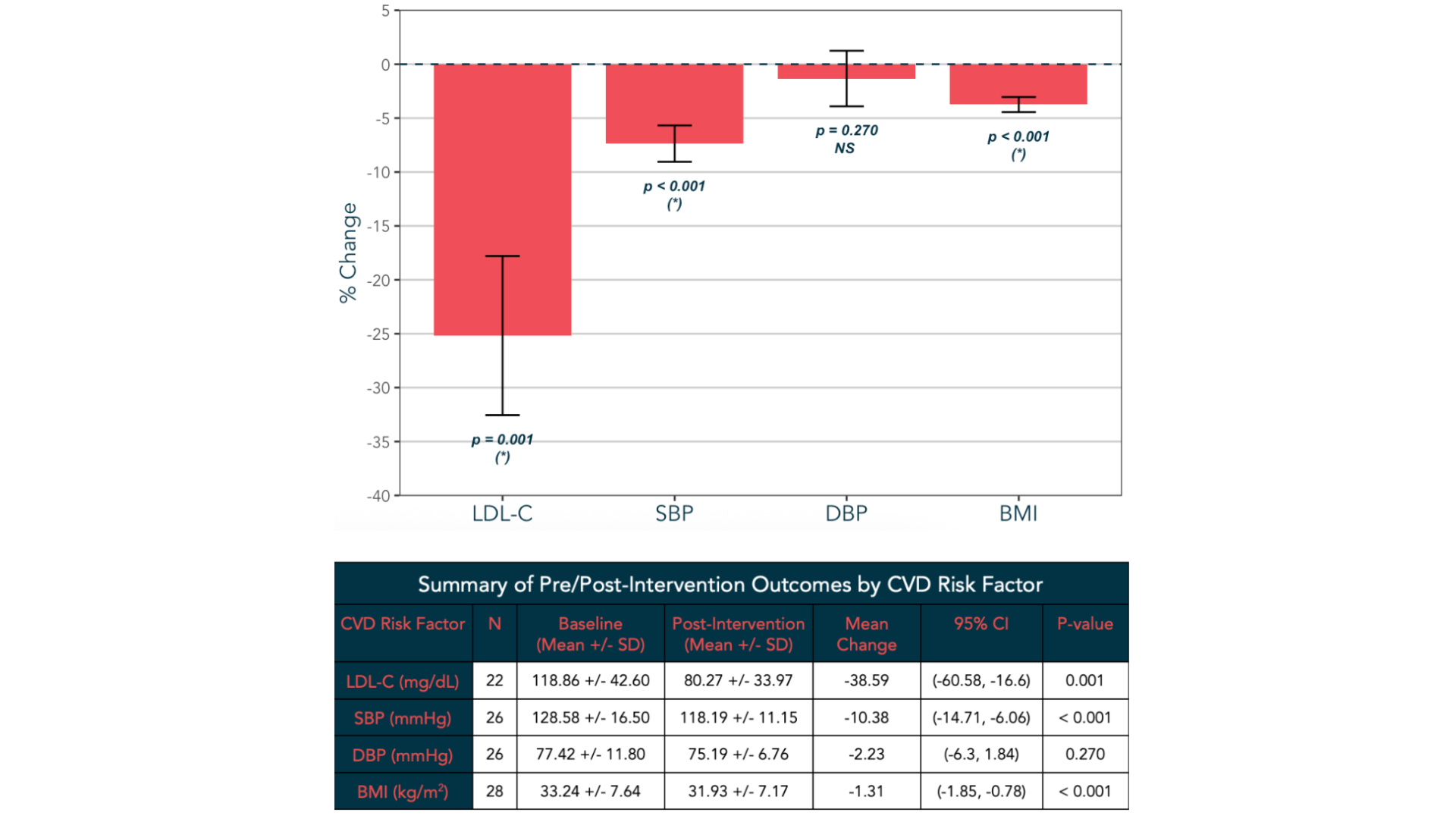
Results: Forty-five women enrolled, contributing 247 patient visits. Mean age was 52 ± 12 years; 87% were White. At baseline, mean systolic BP was 124 ± 15 mmHg, diastolic BP 78 ± 11 mmHg, LDL-C 117 ± 38 mg/dL, and BMI 33.4 ± 7.5 kg/m^2. Most (53%) had ≥3 unoptimized CV risk factors (BP ≥130/80, LDL-C above guideline-recommended thresholds, BMI ≥27, and/or A1c ≥5.7%). Among participants with complete data, mean change in LDL-C was –35.4% (p=0.001), systolic BP –7.0% (p<0.001), diastolic BP -3% (p=0.27), and BMI –4.7% (p<0.001) (Figure 1). Among those receiving medication management (N=20), 36 titrations were performed (mean 1.8 ± 1.5 per patient), with a median intensification time of 8 days (IQR 12.8).
Conclusion: A virtual SMA model for women’s CV health is feasible, scalable, and improves key CV risk factors, offering a promising strategy to close care gaps and reduce population-level CVD risk for women with elevated cardiometabolic risk and/or established CVD.
Introduction: Cardiovascular disease (CVD) is the leading cause of death for women in the United States, yet prevention gaps persist due to provider shortages, underrecognition of sex-specific risk factors, and declining public and professional awareness of the burden of CVD in women. Scalable models that address workforce constraints and enable timely, preventive care for women—such as virtual shared medical appointments—remain poorly defined.
Objective: To evaluate the impact of a virtual shared medical appointment (SMA) model on CV risk factor optimization in women with elevated cardiometabolic risk and/or established CVD.
Methods: Systole Health, a group virtual care organization, enrolled 13 cohorts of 3–5 women into a six-week CV prevention program across 16 U.S. states (April 2024–May 2025). Eligible participants had documented or self-reported overweight/obesity, hypertension (HTN), dyslipidemia (DLD), (pre)diabetes, and/or established CVD. Exclusion criteria included active pregnancy and unstable CVD. The intervention included weekly physician-led SMAs, lifestyle health coaching, and peer support. Medication management was offered to a subset of patients based on clinical need. Outcomes were assessed at baseline and program completion, including self-reported body mass index (BMI), blood pressure (BP) (average of one week of home readings), and LDL cholesterol (LDL-C). Paired two-sample t-tests assessed mean changes.
Results: Forty-five women enrolled, contributing 247 patient visits. Mean age was 52 ± 12 years; 87% were White. At baseline, mean systolic BP was 124 ± 15 mmHg, diastolic BP 78 ± 11 mmHg, LDL-C 117 ± 38 mg/dL, and BMI 33.4 ± 7.5 kg/m^2. Most (53%) had ≥3 unoptimized CV risk factors (BP ≥130/80, LDL-C above guideline-recommended thresholds, BMI ≥27, and/or A1c ≥5.7%). Among participants with complete data, mean change in LDL-C was –35.4% (p=0.001), systolic BP –7.0% (p<0.001), diastolic BP -3% (p=0.27), and BMI –4.7% (p<0.001) (Figure 1). Among those receiving medication management (N=20), 36 titrations were performed (mean 1.8 ± 1.5 per patient), with a median intensification time of 8 days (IQR 12.8).
Conclusion: A virtual SMA model for women’s CV health is feasible, scalable, and improves key CV risk factors, offering a promising strategy to close care gaps and reduce population-level CVD risk for women with elevated cardiometabolic risk and/or established CVD.
More abstracts on this topic:
10-Year Trends in Last Known Well to Arrival Time in Acute Ischemic Stroke Patients: 2014-2023
Ferrone Nicholas, Sanmartin Maria, O'hara Joseph, Jimenez Jean, Ferrone Sophia, Wang Jason, Katz Jeffrey, Sanelli Pina
Accessibility of Vascular Surgeons in Communities at High Risk for Peripheral Artery DiseaseQuinn Patrick, Armstrong Molly, Campbell Drayson, Corriere Matthew