Final ID: MP609
GLP-1 Receptor Agonists and Cardiovascular Outcomes in Patients with Type 2 Diabetes Undergoing TAVI: A Real-World Cohort Study
Abstract Body (Do not enter title and authors here): Introduction: In patients with type 2 diabetes (T2D) at high cardiovascular risk, glucagon-like peptide-1 receptor agonists (GLP1-RAs) have been shown to reduce major adverse cardiovascular events. However, patients with valvular heart disease, including those undergoing transcatheter aortic-valve implantation (TAVI), have been largely excluded from randomized trials.
Hypothesis: We investigated whether GLP1-RA use is associated with improved one-year cardiovascular outcomes in patients with T2D undergoing TAVI.
Methods: We conducted a retrospective cohort study using the TriNetX network. Adults (≥18 years) with T2D who underwent TAVI between 2015 and 2023 were included and stratified based on GLP1-RA initiation within 14 days post-TAVI. Baseline characteristics, comorbidities, medications, and laboratory data were balanced using 1:1 propensity score matching (PSM). The primary outcome was a composite of all-cause mortality or hospitalization at 1 year. Secondary outcomes included acute heart failure (HF) exacerbation, acute myocardial infarction (AMI), cardiac arrest, and ischemic stroke. Outcomes were assessed from 1 month to 1 year after TAVI. Survival probabilities were estimated using Kaplan-Meier analysis, and hazard ratios (HRs) were calculated with Cox proportional hazards models.
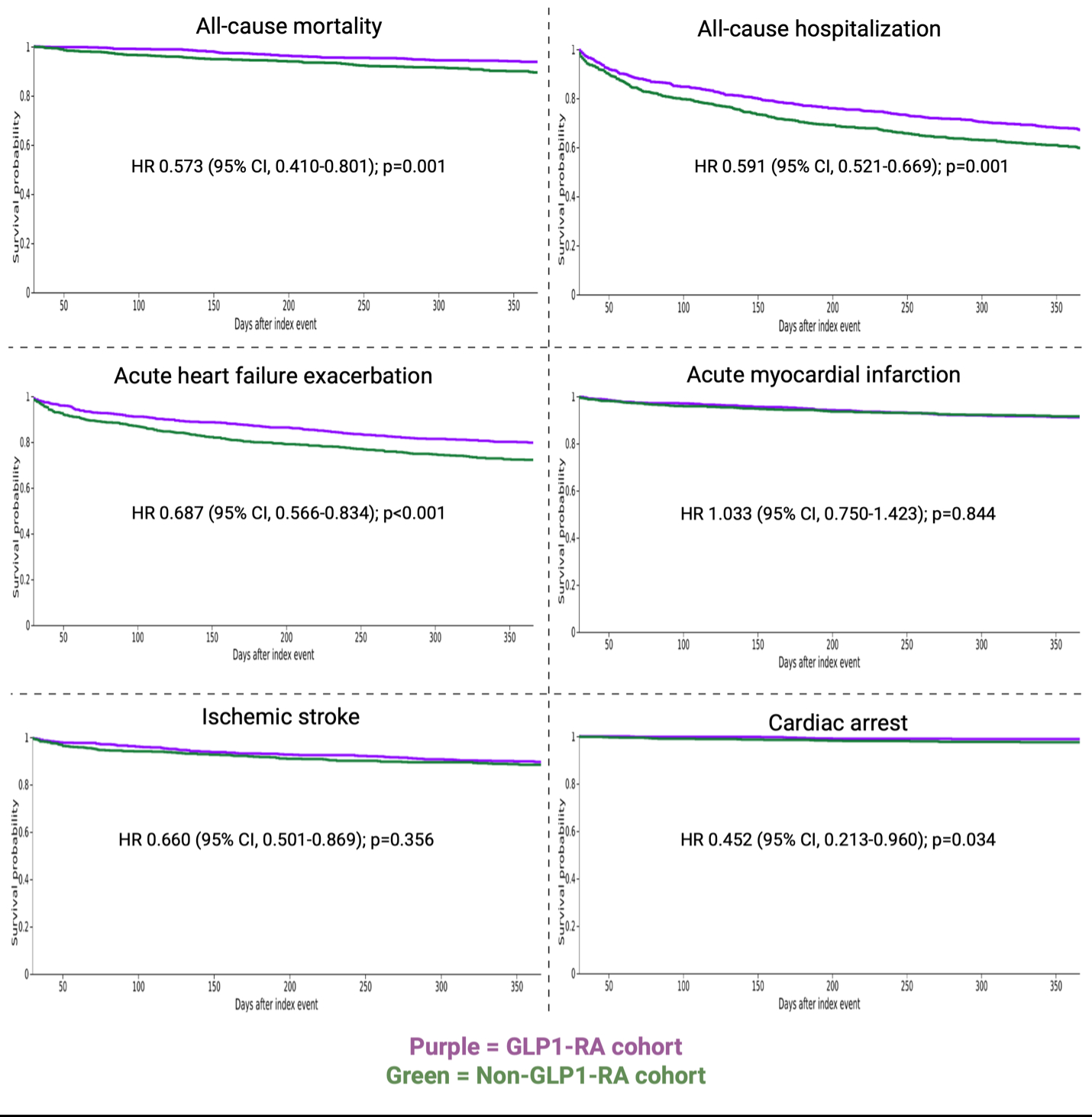
Results: Among 20,454 patients with T2D undergoing TAVI from 2015-2023, 937 received GLP1-RAs. After PSM, 930 patients were included in each cohort, with a mean age of 73 years and 37% female. The mean follow-up duration was 342 days for GLP1-RA users and 325 days for non-users. GLP1-RA cohort exhibited a higher 1-year survival probability (93.8%) compared to non-users (89.5%) (HR 0.573 [95% CI, 0.410-0.801]; p=0.001). GLP1-RA use was also associated lower rates of all-cause hospitalization (HR 0.762 [95% CI, 0.652-0.891]; p=0.001), acute HF exacerbation (HR 0.687 [95% CI, 0.566-0.834]; p<0.001), and cardiac arrest (HR 0.452 [95% CI, 0.213-0.960]; p=0.034). No differences were observed in AMI (HR 1.033 [95% CI, 0.750-1.423]; p=0.844), or ischemic stroke (HR 0.875 [95% CI, 0.659-1.162]; p=0.356).
Conclusions: In patients with T2D undergoing TAVI, GLP1-RA use is associated with significant survival benefits and improved cardiovascular outcomes, including reductions in acute HF exacerbation, all-cause hospitalization, and cardiac arrest. These findings highlight the need for prospective clinical trials to confirm these results.
Hypothesis: We investigated whether GLP1-RA use is associated with improved one-year cardiovascular outcomes in patients with T2D undergoing TAVI.
Methods: We conducted a retrospective cohort study using the TriNetX network. Adults (≥18 years) with T2D who underwent TAVI between 2015 and 2023 were included and stratified based on GLP1-RA initiation within 14 days post-TAVI. Baseline characteristics, comorbidities, medications, and laboratory data were balanced using 1:1 propensity score matching (PSM). The primary outcome was a composite of all-cause mortality or hospitalization at 1 year. Secondary outcomes included acute heart failure (HF) exacerbation, acute myocardial infarction (AMI), cardiac arrest, and ischemic stroke. Outcomes were assessed from 1 month to 1 year after TAVI. Survival probabilities were estimated using Kaplan-Meier analysis, and hazard ratios (HRs) were calculated with Cox proportional hazards models.
Results: Among 20,454 patients with T2D undergoing TAVI from 2015-2023, 937 received GLP1-RAs. After PSM, 930 patients were included in each cohort, with a mean age of 73 years and 37% female. The mean follow-up duration was 342 days for GLP1-RA users and 325 days for non-users. GLP1-RA cohort exhibited a higher 1-year survival probability (93.8%) compared to non-users (89.5%) (HR 0.573 [95% CI, 0.410-0.801]; p=0.001). GLP1-RA use was also associated lower rates of all-cause hospitalization (HR 0.762 [95% CI, 0.652-0.891]; p=0.001), acute HF exacerbation (HR 0.687 [95% CI, 0.566-0.834]; p<0.001), and cardiac arrest (HR 0.452 [95% CI, 0.213-0.960]; p=0.034). No differences were observed in AMI (HR 1.033 [95% CI, 0.750-1.423]; p=0.844), or ischemic stroke (HR 0.875 [95% CI, 0.659-1.162]; p=0.356).
Conclusions: In patients with T2D undergoing TAVI, GLP1-RA use is associated with significant survival benefits and improved cardiovascular outcomes, including reductions in acute HF exacerbation, all-cause hospitalization, and cardiac arrest. These findings highlight the need for prospective clinical trials to confirm these results.
More abstracts on this topic:
Accuracy of cardiologist reporting of severe aortic stenosis and its impact on clinical management: Insights from decision-support artificial intelligence applied to 28,491 men and women undergoing echocardiography.
Bhat Vikas, Strange Geoff, Butcher Steele, Deans Renae, Mahoney Thomas, Barnes Cara, Playford David
Age-Related Differences in Aortic Valve Calcium Progression and the Risk for Aortic Stenosis: Multi-Ethnic Study of AtherosclerosisMarrero Natalie, Thanassoulis George, Rotter Jerome, Blaha Michael, Whelton Seamus, Jha Kunal, Grant Jelani, Razavi Alexander, Budoff Matthew, Shah Sanjiv, Blumenthal Roger, Post Wendy, Shaw Leslee