Final ID: Su3103
Detection and Prognostic Stratification of Left Ventricular Systolic Dysfunction in Left Bundle Branch Block Using an Artificial Intelligence-enabled ECG
Abstract Body (Do not enter title and authors here):
Background
Left bundle branch block (LBBB) significantly increases the risk of left ventricular systolic dysfunction (LVSD) due to cardiac dyssynchrony. While recent advances in artificial intelligence (AI) have enabled ECG-based models to accurately detect LVSD, their performance in LBBB-specific population remains insufficiently validated.
Hypothesis
We hypothesized that AiTiALVSD, a clinically validated AI-ECG model for detecting LVSD, can accurately detect LVSD and predict future risk in LBBB patients.
Methods
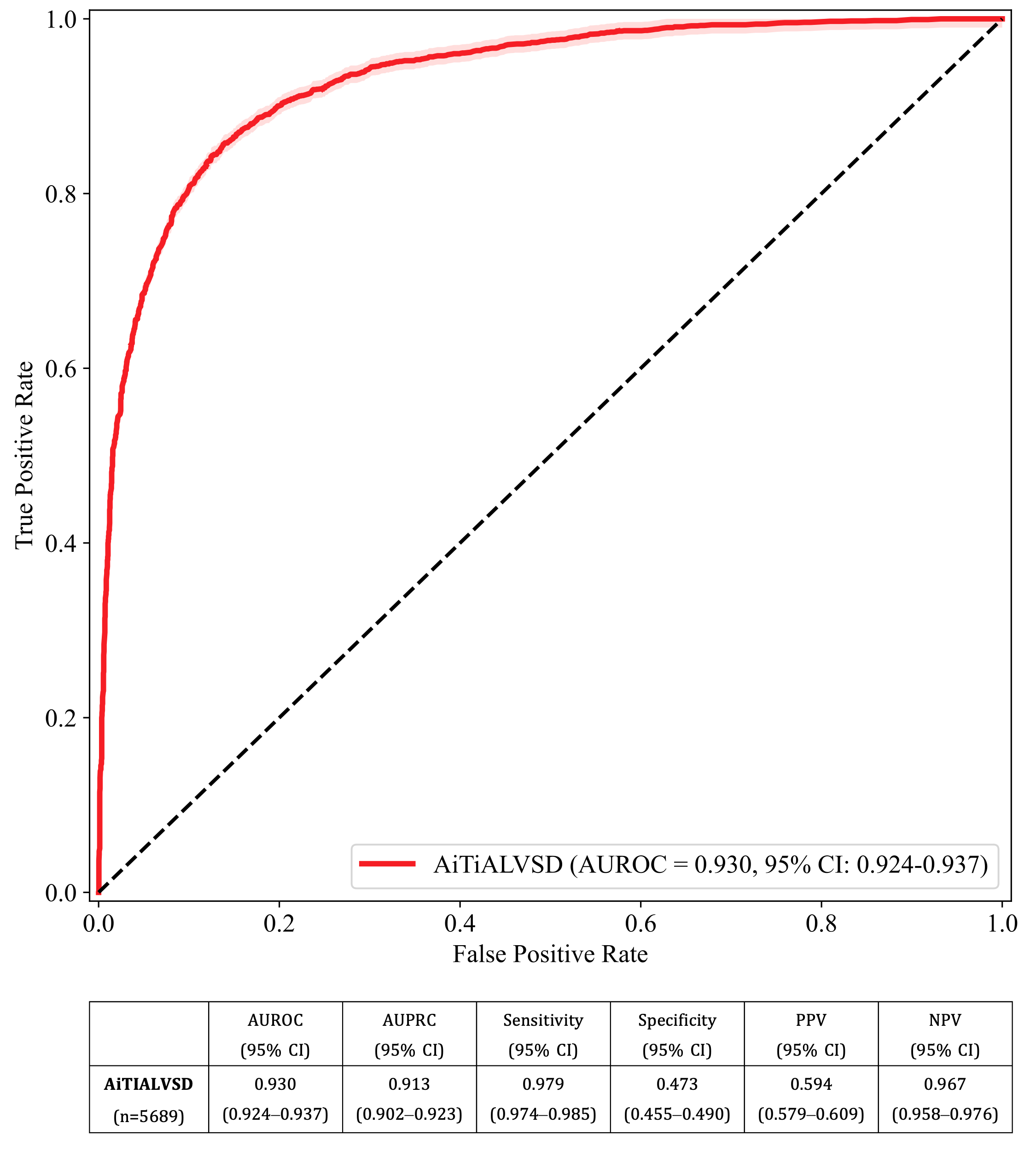
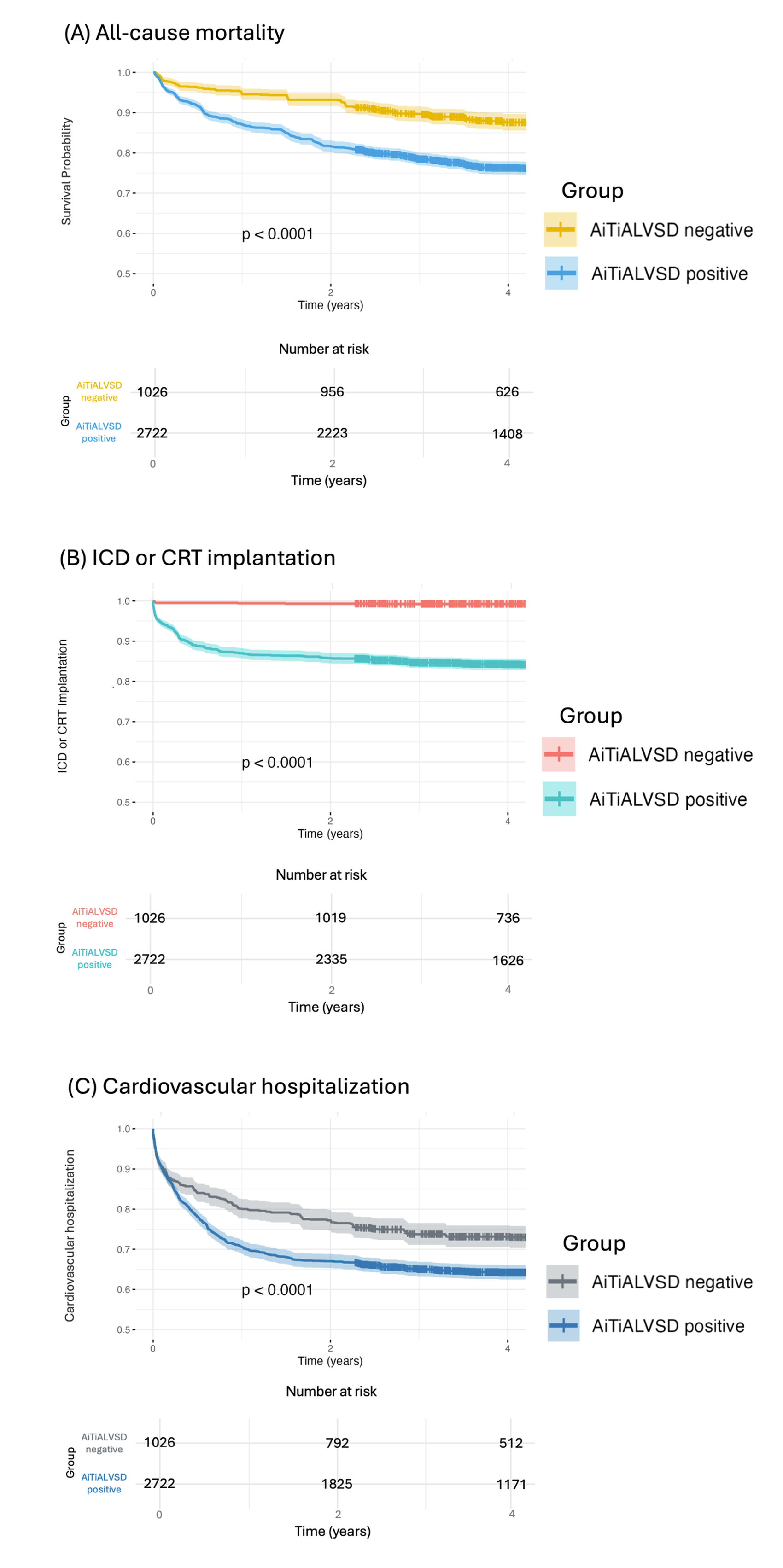
This retrospective multicenter study analyzed 5,689 expert-curated LBBB ECGs of 2,813 patients from two hospitals (2016–2024) using AiTiALVSD V2.00.00 to detect LVSD. Patients with paired ECG and echocardiography within 14 days were included. LBBB was identified through automated screening and expert validation. LVSD was defined as EF ≤40%. Diagnostic performance was evaluated using area under the receiver operating characteristic curve (AUROC), area under precision-recall curve (AUPRC), sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and 95% confidence intervals (CI). Patients were stratified into high- and low-risk groups by AiTiALVSD score, using a predefined threshold to achieve 90% sensitivity. Kaplan–Meier curves were used to assess differences in clinical outcomes between risk groups.
Results
Among 2,813 LBBB patients (mean age 70.7, male 43.7%), hypertension and heart failure were common, and the mean QRS duration was 153.4 ms. The AiTiALVSD model showed strong diagnostic performance for identifying LVSD (AUROC 0.930 [95% CI, 0.924–0.937]; AUPRC 0.913 [95% CI, 0.902–0.923]; sensitivity 0.979 [95% CI, 0.974-0.985]; specificity 0.473 [95%CI, 0.455-0.490]; PPV 0.594 [95% CI, 0.579-0.609]; NPV 0.967 [95%CI, 0.58-0.976]). Mean follow-up duration was 4.1 years. High-risk patients had significantly higher hazards for all-cause mortality (HR 2.29, 95% CI 1.89–2.77), implantable cardioverter defibrillator (ICD)/cardiac resynchronization therapy (CRT) implantation (HR 2.29, 95% CI 1.89–2.77), and cardiovascular hospitalization (HR 1.40, 95% CI 1.22–1.60)(all p values < 0.001).
Conclusion
This multicenter study demonstrates that AiTiALVSD accurately detects LVSD in LBBB patients and effectively stratifies long-term risk for adverse cardiovascular outcomes. These findings support its integration into clinical workflows to enhance early detection and guide proactive management strategies in this high-risk population.
Background
Left bundle branch block (LBBB) significantly increases the risk of left ventricular systolic dysfunction (LVSD) due to cardiac dyssynchrony. While recent advances in artificial intelligence (AI) have enabled ECG-based models to accurately detect LVSD, their performance in LBBB-specific population remains insufficiently validated.
Hypothesis
We hypothesized that AiTiALVSD, a clinically validated AI-ECG model for detecting LVSD, can accurately detect LVSD and predict future risk in LBBB patients.
Methods
This retrospective multicenter study analyzed 5,689 expert-curated LBBB ECGs of 2,813 patients from two hospitals (2016–2024) using AiTiALVSD V2.00.00 to detect LVSD. Patients with paired ECG and echocardiography within 14 days were included. LBBB was identified through automated screening and expert validation. LVSD was defined as EF ≤40%. Diagnostic performance was evaluated using area under the receiver operating characteristic curve (AUROC), area under precision-recall curve (AUPRC), sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and 95% confidence intervals (CI). Patients were stratified into high- and low-risk groups by AiTiALVSD score, using a predefined threshold to achieve 90% sensitivity. Kaplan–Meier curves were used to assess differences in clinical outcomes between risk groups.
Results
Among 2,813 LBBB patients (mean age 70.7, male 43.7%), hypertension and heart failure were common, and the mean QRS duration was 153.4 ms. The AiTiALVSD model showed strong diagnostic performance for identifying LVSD (AUROC 0.930 [95% CI, 0.924–0.937]; AUPRC 0.913 [95% CI, 0.902–0.923]; sensitivity 0.979 [95% CI, 0.974-0.985]; specificity 0.473 [95%CI, 0.455-0.490]; PPV 0.594 [95% CI, 0.579-0.609]; NPV 0.967 [95%CI, 0.58-0.976]). Mean follow-up duration was 4.1 years. High-risk patients had significantly higher hazards for all-cause mortality (HR 2.29, 95% CI 1.89–2.77), implantable cardioverter defibrillator (ICD)/cardiac resynchronization therapy (CRT) implantation (HR 2.29, 95% CI 1.89–2.77), and cardiovascular hospitalization (HR 1.40, 95% CI 1.22–1.60)(all p values < 0.001).
Conclusion
This multicenter study demonstrates that AiTiALVSD accurately detects LVSD in LBBB patients and effectively stratifies long-term risk for adverse cardiovascular outcomes. These findings support its integration into clinical workflows to enhance early detection and guide proactive management strategies in this high-risk population.
More abstracts on this topic:
A Case of Steroid-Refractory Immune-checkpoint-inhibitor Induced Myocarditis Responsive to Mycophenolate and Anti-thymocyte globulin
Dabdoub Jorge, Wilson Michael, Gottbrecht Matthew, Salazar Ryan, Shih Jeffrey
A Deep Learning Digital Biomarker for Mitral Valve Prolapse using Echocardiogram VideosAl-alusi Mostafa, Khurshid Shaan, Sanborn Danita, Picard Michael, Ho Jennifer, Maddah Mahnaz, Ellinor Patrick, Lau Emily, Small Aeron, Reeder Christopher, Shnitzer Dery Tal, Andrews Carl, Kany Shinwan, Ramo Joel, Haimovich Julian