Final ID: MP905
Glucagon-like-peptide-1 Receptor Agonists Are Associated with Lower Postoperative Complication Rates in Patients with Peripheral Artery Disease
Abstract Body (Do not enter title and authors here): Introduction: The American Diabetes Association recommends use of glucagon-like-peptide-1 receptor agonists (GLP-1RAs) by patients with peripheral arterial disease (PAD) despite limited information regarding the impact of GLP-1RAs in these patients.
Hypothesis: Patients using GLP-1RAs have lower rates of adverse events following revascularization.
Methods: Our retrospective cohort (18-hospital, unified health care system; 2016-2024) included diabetic adults undergoing an index PAD revascularization, stratified by GLP-1RAs prescription. The primary outcome was overall mortality. Secondary outcomes included major adverse limb events (MALE), major adverse cardiac events (MACE), major amputation, and acute coronary syndromes (ACS). Outcomes were compared via Kaplan Meier analysis and entropy-balanced Cox regression using demographic, medical, healthy user parameters, intervention, and facility factors generating adjusted hazard ratios (aHR) and 95% confidence intervals (CI).
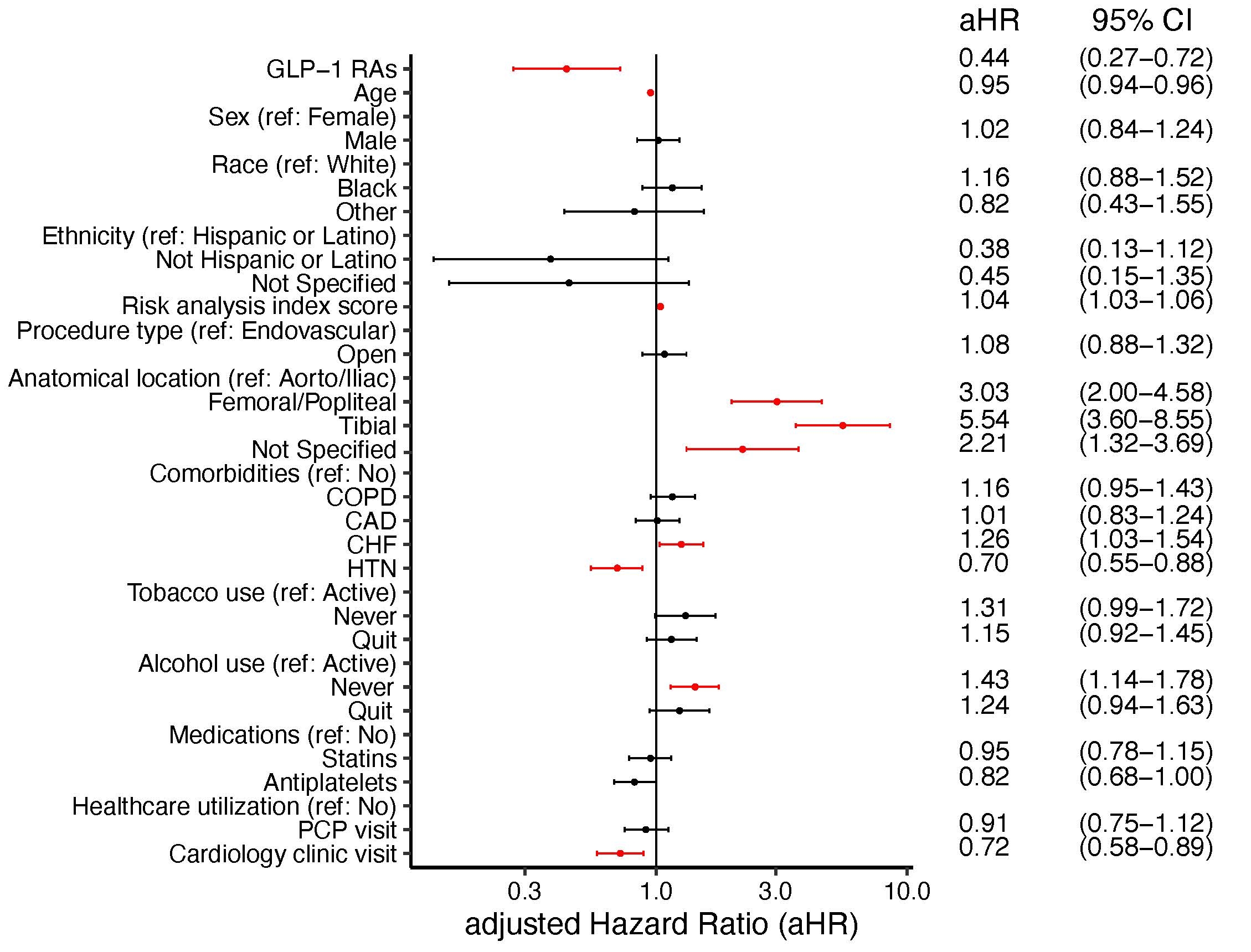
Results: We included 5,008 patients (age 69±11 years; 1,858 [37.1%] females; 4,400 [87.8%] White; 1,766 [35.2%] open interventions) of which 468 (9.3%) were prescribed GLP-1RAs. On unadjusted analysis, GLP-1RAs prescriptions were correlated with lower mortality rates (60 [13%] vs 1,649 [36%], p<0.001) (Figure 1) and ACS events (42 [9%] vs 642 [14%], p=0.04). However, MALE (123 [26%] vs 1,306 [29%], p=0.45), MACE (81 [17%] vs1,048 [23%], p=0.18), and major amputation (38 [8%] vs 498 [11%], p=0.12) differences were non-significant. After entropy-balance, covariates were well balanced with all standardized mean differences <0.1. Entropy-balance and multivariable regression noted GLP-1RA prescriptions were associated with a reduced risk of mortality (aHR [95%CI]: 0.65 [0.44-0.96]), ACS (aHR [95%CI]: 0.61 [0.37-0.99]), and major amputation (aHR [95%CI]: 0.45 [0.28-0.73]) (Figure 2) but failed to reach significance for MALE (aHR [95%CI]: 0.76 [0.56-1.03]) and MACE (aHR [95%CI]: 0.89 [0.61-1.30]).
Conclusions: GLP-1RAs use in diabetic patients undergoing revascularization for PAD was associated with significantly decreased rates of postoperative mortality, major amputation, and ACS events after lower extremity revascularization. These findings support the benefit of these medications in the diabetic PAD population and warrant further investigation to understand mechanism of protection of these medications and the potential expanded use in nondiabetic patients with PAD.
Hypothesis: Patients using GLP-1RAs have lower rates of adverse events following revascularization.
Methods: Our retrospective cohort (18-hospital, unified health care system; 2016-2024) included diabetic adults undergoing an index PAD revascularization, stratified by GLP-1RAs prescription. The primary outcome was overall mortality. Secondary outcomes included major adverse limb events (MALE), major adverse cardiac events (MACE), major amputation, and acute coronary syndromes (ACS). Outcomes were compared via Kaplan Meier analysis and entropy-balanced Cox regression using demographic, medical, healthy user parameters, intervention, and facility factors generating adjusted hazard ratios (aHR) and 95% confidence intervals (CI).
Results: We included 5,008 patients (age 69±11 years; 1,858 [37.1%] females; 4,400 [87.8%] White; 1,766 [35.2%] open interventions) of which 468 (9.3%) were prescribed GLP-1RAs. On unadjusted analysis, GLP-1RAs prescriptions were correlated with lower mortality rates (60 [13%] vs 1,649 [36%], p<0.001) (Figure 1) and ACS events (42 [9%] vs 642 [14%], p=0.04). However, MALE (123 [26%] vs 1,306 [29%], p=0.45), MACE (81 [17%] vs1,048 [23%], p=0.18), and major amputation (38 [8%] vs 498 [11%], p=0.12) differences were non-significant. After entropy-balance, covariates were well balanced with all standardized mean differences <0.1. Entropy-balance and multivariable regression noted GLP-1RA prescriptions were associated with a reduced risk of mortality (aHR [95%CI]: 0.65 [0.44-0.96]), ACS (aHR [95%CI]: 0.61 [0.37-0.99]), and major amputation (aHR [95%CI]: 0.45 [0.28-0.73]) (Figure 2) but failed to reach significance for MALE (aHR [95%CI]: 0.76 [0.56-1.03]) and MACE (aHR [95%CI]: 0.89 [0.61-1.30]).
Conclusions: GLP-1RAs use in diabetic patients undergoing revascularization for PAD was associated with significantly decreased rates of postoperative mortality, major amputation, and ACS events after lower extremity revascularization. These findings support the benefit of these medications in the diabetic PAD population and warrant further investigation to understand mechanism of protection of these medications and the potential expanded use in nondiabetic patients with PAD.
More abstracts on this topic:
Adverse Pregnancy Outcomes Are Associated with Incident Peripheral Artery Disease, Results from the Women’s Health Initiative.
Jackson Elizabeth, Leblanc Erin, Haring Bernhard, Harrington Laura, Allison Matthew, Eaton Charles, Lamonte Michael, Hovey Kathleen, Andrews Chris, Wells Gretchen, Manson Joann, Levitan Emily, Spracklen Cassandra, Wild Robert
Aspirin for Primary Prevention of Cardiovascular Events in Patients with Diabetes Mellitus: An Updated Systematic Review, Meta-Analysis & Trial Sequential Analysis of Randomized Controlled Trials post-ASCEND TrialPuthia Valappil Omer Mohammed, John M Rose, Mallikarjun Samanth, D Souza Leroy, Rongala Sai Anurag, Chakraborty Diya, Balarishnan Rojith, Kutty Shelby