Final ID: Mo4078
Antihistamine Treatment to Reduce Microvascular Obstruction and Hemorrhage in Reperfused Myocardial Infarction
Abstract Body (Do not enter title and authors here): Purpose: While mast cells (MCs) have been shown to exacerbate damage in hemorrhagic stroke models by amplifying histamine-driven inflammation, disrupting the blood-brain barrier and promoting hemorrhage, their role in reperfused myocardial infarction (MI) remains unclear. It has been long known that reperfusion after prolonged ischemia worsens myocardial injury by inducing inflammation, microvascular obstruction (MVO) and intramyocardial hemorrhage (IMH). This process involves erythrocyte and neutrophil-platelet aggregation, releasing inflammatory mediators that increase vasoconstriction, edema, and intravascular pressure, leading to microvascular rupture and IMH. We hypothesized that MC stabilization reduces MVO and IMH post-reperfusion.
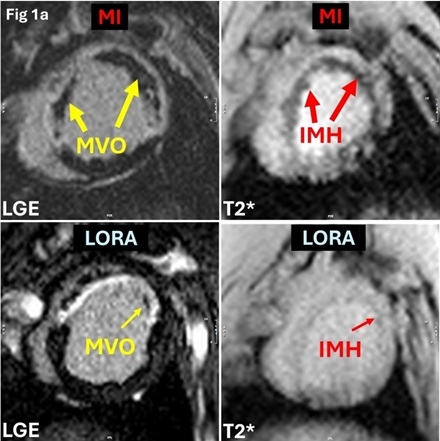
Methods: Female farm pigs (n=24; 30-35kg) underwent a 90-minute occlusion of left anterior descending artery followed by reperfusion to induce MVO. Animals were randomized into untreated MI (MI; n=12) and loratadine-treated (LORA; n=12) groups, with the latter receiving oral loratadine (10mg/day) for 5 days; after which infarcts were assessed for IMH and MVO (Figure 1a). Non-infarcted animals of the same initial weight were used as control (CTRL; n=10) group. On Day 5 post-MI, clinical 3T scanner was used to acquire cine, LGE and T2* CMR.
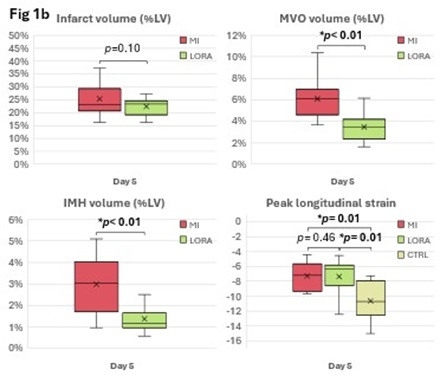
Results: At Day 5 post-MI, there was no significant difference in infarct size between untreated MI (25.39±6.78%LV) and LORA (22.41±3.74%LV; p=0.10) groups. End systolic volume (ESV), end diastolic volume (EDV) and peak global longitudinal strain (PLS) were not significantly different between LORA (ESV: 63.84±11.96ml; EDV: 98.52±15.62ml; PLS: -7.36±2.20) and untreated MI (ESV: 60.16±15.56ml, p=0.27; EDV: 98.51±16.24ml, p=0.50; PLS: -7.26±1.92, p=0.46). ESV and EDV in both LORA (p<0.01) and untreated MI (p<0.01) were significantly higher compared to CTRL (ESV: 31.36±6.28ml; EDV: 60.11±7.51ml), PLS was significantly decreased in LORA (p=0.01) and untreated MI (p=0.01) compared to CTRL (PLS: -10.62±2.65). Notably, LORA showed reduced MVO (3.49±1.31%LV vs. 6.10±1.92%LV, p<0.01) and IMH (1.37±0.58%LV vs. 2.98±1.20%LV, p<0.01) versus untreated MI (Figures 1a-b).
Conclusions: Loratadine treatment significantly attenuated MVO and IMH in acute MI post-reperfusion, suggesting its potential as a pharmacological intervention in acute MI. It remains to be determined whether short-term antihistamine administration translates into beneficial cardiac remodelling during the chronic phase.
Methods: Female farm pigs (n=24; 30-35kg) underwent a 90-minute occlusion of left anterior descending artery followed by reperfusion to induce MVO. Animals were randomized into untreated MI (MI; n=12) and loratadine-treated (LORA; n=12) groups, with the latter receiving oral loratadine (10mg/day) for 5 days; after which infarcts were assessed for IMH and MVO (Figure 1a). Non-infarcted animals of the same initial weight were used as control (CTRL; n=10) group. On Day 5 post-MI, clinical 3T scanner was used to acquire cine, LGE and T2* CMR.
Results: At Day 5 post-MI, there was no significant difference in infarct size between untreated MI (25.39±6.78%LV) and LORA (22.41±3.74%LV; p=0.10) groups. End systolic volume (ESV), end diastolic volume (EDV) and peak global longitudinal strain (PLS) were not significantly different between LORA (ESV: 63.84±11.96ml; EDV: 98.52±15.62ml; PLS: -7.36±2.20) and untreated MI (ESV: 60.16±15.56ml, p=0.27; EDV: 98.51±16.24ml, p=0.50; PLS: -7.26±1.92, p=0.46). ESV and EDV in both LORA (p<0.01) and untreated MI (p<0.01) were significantly higher compared to CTRL (ESV: 31.36±6.28ml; EDV: 60.11±7.51ml), PLS was significantly decreased in LORA (p=0.01) and untreated MI (p=0.01) compared to CTRL (PLS: -10.62±2.65). Notably, LORA showed reduced MVO (3.49±1.31%LV vs. 6.10±1.92%LV, p<0.01) and IMH (1.37±0.58%LV vs. 2.98±1.20%LV, p<0.01) versus untreated MI (Figures 1a-b).
Conclusions: Loratadine treatment significantly attenuated MVO and IMH in acute MI post-reperfusion, suggesting its potential as a pharmacological intervention in acute MI. It remains to be determined whether short-term antihistamine administration translates into beneficial cardiac remodelling during the chronic phase.
More abstracts on this topic:
A Framework for Developing Prehospital Intracerebral Hemorrhage Recognition Scales and Technologies
Taleb Shayandokht, Hsu Jamie, Saver Jeffrey
Angio-IMR - A Novel Angiography-Derived Index of Microcirculatory Resistance for Assessment of Coronary Microvascular DysfunctionO'brien Joseph, Ford Tom, Wong Dennis, Zhang Jun Michael, Yong Andy, Easey Kelly, Redwood Eleanor, Rehan Rajan, Ravindran Jayant, Brown Adam, Chew Derek