Final ID: MP1162
Mast Cell Stabilization Enhances Hemorrhage Resolution and Attenuates Adverse Remodeling in Reperfused Myocardial Infarction
Abstract Body (Do not enter title and authors here): Purpose: Evidence suggests that mast cells (MCs) become overstimulated during reperfusion after a period of prolonged myocardial ischemia. However, the role of MC degranulation on post-reperfusion hemorrhage formation/resolution is unknown. Notably, recent in vitro studies have shown that, as opposed to resting/unstimulated MCs, activated MCs act as "scavengers" by actively engulfing and clearing damaged/oxidized erythrocytes (oxRBC). To date, however, the interaction of MCs with stagnant blood/oxydized erythrocytes in reperfused infarcted myocardium (MI) remains grossly unexplored. In the present study, we investigated the effects of MC stabilization on post-MI hemorrhage resorption/clearance in a clinically relevant porcine model using longitudinal MRI.
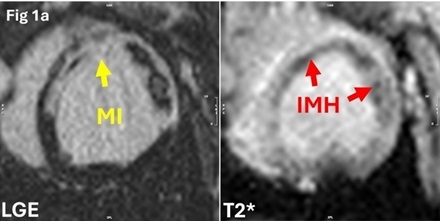
Methods: Female farm pigs (n=14; 30-35kg) underwent 90-minute occlusion of the left anterior descending artery followed by reperfusion. At Day 5, MI and intramyocardial hemorrhage (IMH) were confirmed using a clinical 3T MRI scanner (Figure 1a). Pigs with comparable MI, IMH and microvascular obstruction (MVO) sizes were randomized into untreated MI (MI, n=7) and treated (LORA, n=7) groups, with the latter given daily oral loratadine (10mg) until termination. The animals were followed longitudinally through Weeks 4 and 8. Cardiac function was assessed using cine MRI sequences (short-axis, horizontal, and vertical long-axis). MI and MVO were quantified using LGE, while IMH was assessed using T2*-weighted imaging.
Results: As seen in Figure 1b, no significant differences were observed in infarct (p=0.23), MVO (p=0.21) or IMH (p=0.11) sizes between the untreated MI and LORA groups at Day 5. Hemorrhage resorption from Day 5 to Week 4 and Week 8 was significantly greater in LORA (Week 4: -89.37%; Week 8: -96.53%) than in untreated MI (Week 4: -73.67%, p<0.05; Week 8: -88.66%, p=0.02). Notably, at Week 8, while both groups demonstrated similar (p=0.48) reductions in MI scar size, the extent of ventricle volume increase was significantly lower in LORA (ESV: +22.23%; EDV: +25.06%) compared to untreated MI (ESV: +64.55%, p<0.01; EDV: +64.11%, p=0.02) group.
Conclusions: MC stabilization accelerates hemorrhage resolution and attenuates adverse remodeling in hemorrhagic MI. However, whether overstimulated MC during myocardial ischemia/reperfusion directly exhibit reduced oxRBC scavenging potential, or it is the MC degranulation that indirectly inhibits hemorrhage resolution, remains to be determined.
Methods: Female farm pigs (n=14; 30-35kg) underwent 90-minute occlusion of the left anterior descending artery followed by reperfusion. At Day 5, MI and intramyocardial hemorrhage (IMH) were confirmed using a clinical 3T MRI scanner (Figure 1a). Pigs with comparable MI, IMH and microvascular obstruction (MVO) sizes were randomized into untreated MI (MI, n=7) and treated (LORA, n=7) groups, with the latter given daily oral loratadine (10mg) until termination. The animals were followed longitudinally through Weeks 4 and 8. Cardiac function was assessed using cine MRI sequences (short-axis, horizontal, and vertical long-axis). MI and MVO were quantified using LGE, while IMH was assessed using T2*-weighted imaging.
Results: As seen in Figure 1b, no significant differences were observed in infarct (p=0.23), MVO (p=0.21) or IMH (p=0.11) sizes between the untreated MI and LORA groups at Day 5. Hemorrhage resorption from Day 5 to Week 4 and Week 8 was significantly greater in LORA (Week 4: -89.37%; Week 8: -96.53%) than in untreated MI (Week 4: -73.67%, p<0.05; Week 8: -88.66%, p=0.02). Notably, at Week 8, while both groups demonstrated similar (p=0.48) reductions in MI scar size, the extent of ventricle volume increase was significantly lower in LORA (ESV: +22.23%; EDV: +25.06%) compared to untreated MI (ESV: +64.55%, p<0.01; EDV: +64.11%, p=0.02) group.
Conclusions: MC stabilization accelerates hemorrhage resolution and attenuates adverse remodeling in hemorrhagic MI. However, whether overstimulated MC during myocardial ischemia/reperfusion directly exhibit reduced oxRBC scavenging potential, or it is the MC degranulation that indirectly inhibits hemorrhage resolution, remains to be determined.
More abstracts on this topic:
A Blood(y) Pressure Crisis: Diffuse Alveolar Hemorrhage as a Rare Manifestation of Severely Uncontrolled Hypertension
Nandyal Shreyas, Amdetsion Gedion Yilma, Varma Revati, Kohli Saksham, Hammo Hasan
A New Neurological Assessment Focused on Consciousness and Quantitative Motor Function in a Rat Model of Subarachnoid HemorrhageKanamaru Hideki, Zhu Shiyi, Han Mingyang, Huang Lei, Sherchan Prativa, Suzuki Hidenori, Tang Jiping, Zhang John