Final ID: Mo3133
Association Between Pre-Operative History of Significant Bleeding and Post-Operative Cardiovascular Events Following Lower Extremity Revascularization
Abstract Body (Do not enter title and authors here): Background and Hypothesis: Patients with symptomatic peripheral artery disease (PAD) frequently undergo lower extremity revascularization (LER) but remain at increased risk of major adverse cardiovascular and limb events following the procedure. Patients with a bleeding history tend to have lower platelet activity and thus may be at lower risk for a cardiovascular event following LER.
Methods/Approach: Patients aged ≥21 years and scheduled for non-emergent LER were recruited for participation. Based on self-reported history of seven types of significant bleeding (significant nosebleeds, hematuria, gastrointestinal bleeding, oral cavity bleeding, bleeding after surgery or major trauma, and non-trauma related central nervous system or ocular bleeding), 289 participants with complete information were stratified into three groups: no history of significant bleeding (186, 64%), history of significant bleeding not requiring medical attention (48, 17%), and history of significant bleeding requiring medical attention (55, 19%).
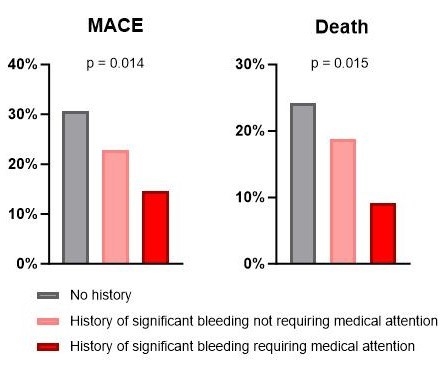
Results: There were no differences between groups observed in age, sex, race, ethnicity, diabetes, hypertension and prior coronary artery disease. Body mass index was lowest in the no-history group, higher in the non-medical-attention group, and highest in the medical-attention group (26.2, 27.8, 28.1 kg/m2, respectively; p=0.012). After a median follow-up of 18 months, a composite of major adverse cardiovascular events (MACE; death, myocardial infarction, and stroke) and death occurred in 26.3% and 20.4% of all participants, respectively. History of bleeding was associated with improved clinical outcomes, with MACE and death occurring less frequently in the non-medical-attention group and less frequently still in the medical-attention group. MACE occurred in 30.6%, 22.9%, and 14.5% of participants in the no-history, non-medical-attention, and medical-attention groups, respectively (Figure 1, p = 0.014). Death occurred in 24.2%, 18.8%, and 9.1% of participants in the no-history, non-medical-attention, and medical-attention groups, respectively (Figure 1, p = 0.015).
Conclusion: Pre-operative history of bleeding exhibits a relationship with adverse outcomes following LER. Participants with a history of significant bleeding, especially significant bleeding requiring medical attention, experience lower risk of MACE and death.
Methods/Approach: Patients aged ≥21 years and scheduled for non-emergent LER were recruited for participation. Based on self-reported history of seven types of significant bleeding (significant nosebleeds, hematuria, gastrointestinal bleeding, oral cavity bleeding, bleeding after surgery or major trauma, and non-trauma related central nervous system or ocular bleeding), 289 participants with complete information were stratified into three groups: no history of significant bleeding (186, 64%), history of significant bleeding not requiring medical attention (48, 17%), and history of significant bleeding requiring medical attention (55, 19%).
Results: There were no differences between groups observed in age, sex, race, ethnicity, diabetes, hypertension and prior coronary artery disease. Body mass index was lowest in the no-history group, higher in the non-medical-attention group, and highest in the medical-attention group (26.2, 27.8, 28.1 kg/m2, respectively; p=0.012). After a median follow-up of 18 months, a composite of major adverse cardiovascular events (MACE; death, myocardial infarction, and stroke) and death occurred in 26.3% and 20.4% of all participants, respectively. History of bleeding was associated with improved clinical outcomes, with MACE and death occurring less frequently in the non-medical-attention group and less frequently still in the medical-attention group. MACE occurred in 30.6%, 22.9%, and 14.5% of participants in the no-history, non-medical-attention, and medical-attention groups, respectively (Figure 1, p = 0.014). Death occurred in 24.2%, 18.8%, and 9.1% of participants in the no-history, non-medical-attention, and medical-attention groups, respectively (Figure 1, p = 0.015).
Conclusion: Pre-operative history of bleeding exhibits a relationship with adverse outcomes following LER. Participants with a history of significant bleeding, especially significant bleeding requiring medical attention, experience lower risk of MACE and death.
More abstracts on this topic:
Acute Left Ventricular Thrombosis and Systemic Embolism Following Testosterone Therapy
Rasheed Ahmed Daniyaal, Naseer Ahmed, Nadig Vidya
A Non-odorant Olfactory Receptor Ligand Depolymerizes the Platelet Actin Cytoskeleton to Prevent ThrombosisAggarwal Anu, Godwin Matthew, Ali Mariya, Jennings Courtney, Rajasekar Bhairavi, Scalise Alliefair, Stauffer Shaun, Mccrae Keith, Mcintyre Thomas, Cameron Scott, Wang Nancy, Josyula Vara Prasad, Yang Moua, Young Shim, Kennedy Quinn, Samuel Reina, Sangwan Naseer, Guntupalli Suman