Final ID: MP1727
Contemporary Management and Outcomes of Newly Diagnosed Chronic Limb Threatening Ischemia in the Veterans Affairs Health Care System
Abstract Body (Do not enter title and authors here): Introduction: Chronic limb threatening ischemia (CLTI) is associated with high risks of amputation and mortality. The purpose of this study was to investigate the patterns of management of patients with new onset CLTI in the Veterans Affairs Health Care System.
Methods: We identified patients with new-onset peripheral artery disease (PAD), defined by ankle-brachial index (ABI) <0.9, from 2015-2020 who progressed to CLTI, based on ICD codes, before the year 2024, within a longitudinal registry of PAD among Veterans (Peripheral Artery Disease: Long-term Survival Study – PEARLS). The main exposure was revascularization (surgical or endovascular) within 6 months of CLTI diagnosis. A Cox proportion hazards model examined the association between revascularization and the composite endpoint of death and major amputation, adjusted for demographics, PAD severity, smoking status, and comorbidities.
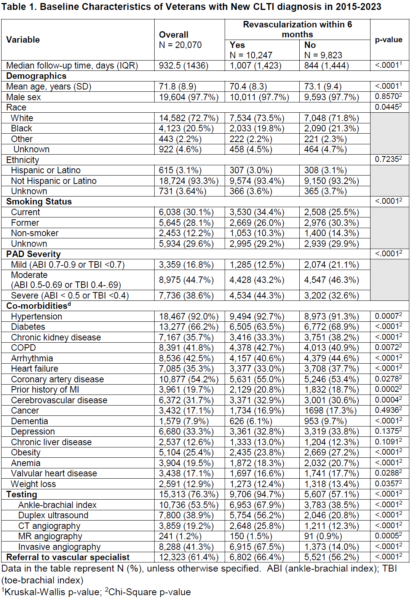
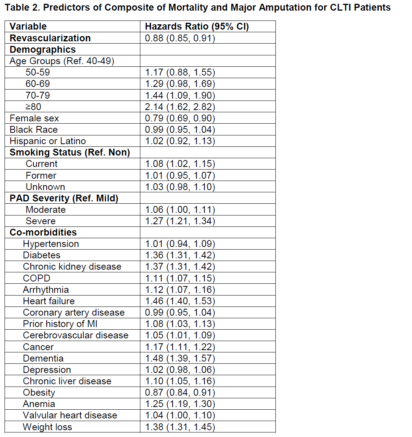
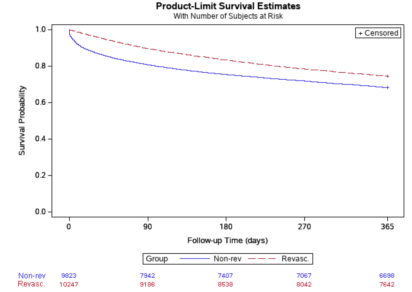
Results: Among 20,070 patients with newly diagnosed CLTI, 10,247 (51.1%) underwent revascularization (27% surgical, 73% endovascular) within 6 months. Compared to patients who did not undergo revascularization (non-revascularization group), patients in the revascularization group were younger, more likely to be active smokers, and have severe PAD (Table 1). Overall, 76.3% underwent additional diagnostic studies following CLTI diagnosis and 61.4% were referred to a vascular specialist; both rates were higher in the revascularization compared to the non-revascularization group (Table 1). The median time to revascularization was 4 days. At 1 year, patients in the revascularization group had lower rates of major amputation (12.2% vs. 14.6%), mortality (16.0% vs. 21.2%) and higher amputation free survival (74.6% vs. 68.2%) (Figure). Among those with major amputation (3821 [19.0%]), median time to amputation was longer in the revascularization group (207 days vs. 29 days). Based on the adjusted cox proportional hazard model, age >80, diabetes, chronic kidney disease, heart failure and weight loss were associated with higher risk of death or major amputation, whereas revascularization was significantly associated with a lower hazard ratio for the composite endpoint (Table 2).
Conclusion: Among Veterans with new CLTI, more than 75% receive additional diagnostic evaluation, 60% are referred to a vascular specialist, and 1 in 2 undergo revascularization. Although revascularization is associated with improved outcomes, the overall rate of major amputation and mortality remains high.
Methods: We identified patients with new-onset peripheral artery disease (PAD), defined by ankle-brachial index (ABI) <0.9, from 2015-2020 who progressed to CLTI, based on ICD codes, before the year 2024, within a longitudinal registry of PAD among Veterans (Peripheral Artery Disease: Long-term Survival Study – PEARLS). The main exposure was revascularization (surgical or endovascular) within 6 months of CLTI diagnosis. A Cox proportion hazards model examined the association between revascularization and the composite endpoint of death and major amputation, adjusted for demographics, PAD severity, smoking status, and comorbidities.
Results: Among 20,070 patients with newly diagnosed CLTI, 10,247 (51.1%) underwent revascularization (27% surgical, 73% endovascular) within 6 months. Compared to patients who did not undergo revascularization (non-revascularization group), patients in the revascularization group were younger, more likely to be active smokers, and have severe PAD (Table 1). Overall, 76.3% underwent additional diagnostic studies following CLTI diagnosis and 61.4% were referred to a vascular specialist; both rates were higher in the revascularization compared to the non-revascularization group (Table 1). The median time to revascularization was 4 days. At 1 year, patients in the revascularization group had lower rates of major amputation (12.2% vs. 14.6%), mortality (16.0% vs. 21.2%) and higher amputation free survival (74.6% vs. 68.2%) (Figure). Among those with major amputation (3821 [19.0%]), median time to amputation was longer in the revascularization group (207 days vs. 29 days). Based on the adjusted cox proportional hazard model, age >80, diabetes, chronic kidney disease, heart failure and weight loss were associated with higher risk of death or major amputation, whereas revascularization was significantly associated with a lower hazard ratio for the composite endpoint (Table 2).
Conclusion: Among Veterans with new CLTI, more than 75% receive additional diagnostic evaluation, 60% are referred to a vascular specialist, and 1 in 2 undergo revascularization. Although revascularization is associated with improved outcomes, the overall rate of major amputation and mortality remains high.
More abstracts on this topic:
3D spheroids composed by induced Skeletal Muscle Progenitor Cells and Mesenchymal Stem Cells derived from human Pluripotent Stem Cells can recapitulate embryonic niches in hindlimb ischemia model
Kim Jinju, Park Jae-hyun, Choi Yeon-jik, Park Hun
24-Dehydrocholesterol Reductase Plays a Significant Role in Inflammation During Peripheral Arterial DiseaseLassance-soares Roberta, Falero-diaz Gustavo, Montoya Christopher, Barboza Catarina