Final ID: MP2402
Chronotropic Incompetence Predicts Reduced Survival and Exercise Capacity in Heart Failure: A Meta-Analysis of Reconstructed Time-to-Event Data Across HFrEF and HFpEF
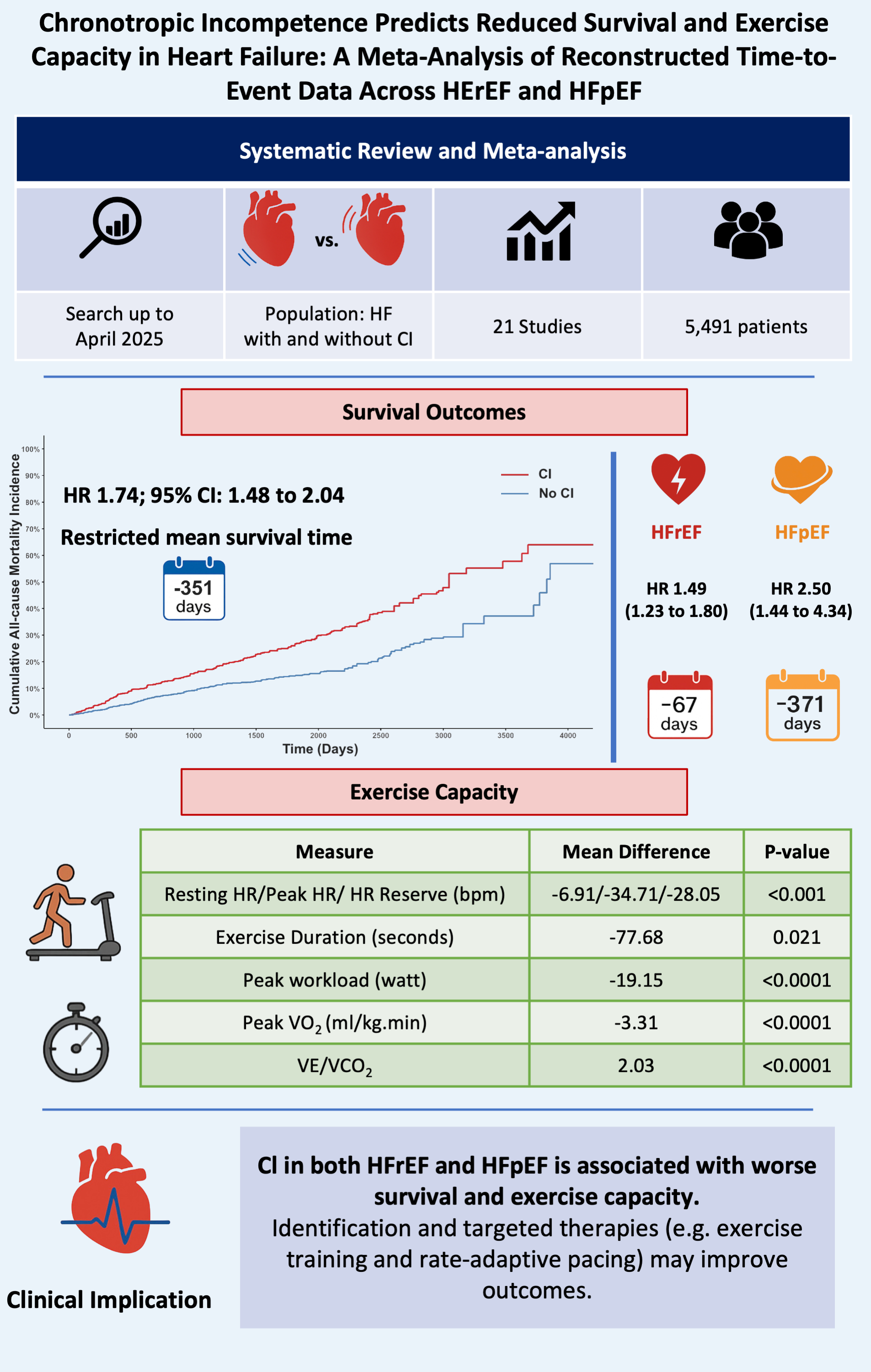
Abstract Body (Do not enter title and authors here): Background: Chronotropic incompetence (CI) is the inability of the heart to increase its rate adequately during activity. It is common in heart failure (HF) patients and is associated with poorer exercise capacity and clinical outcomes. This study systematically examines prognosis and functional outcomes in HF patients with and without CI.
Method: We searched PubMed, Embase, Scopus, and the Cochrane Library for studies published up to April 8, 2025, comparing overall survival and exercise performance in HF patients with and without CI. All-cause mortality was assessed using Cox proportional hazards models based on reconstructed individual patient data. Exercise performance differences were analyzed as mean differences (MD) using the DerSimonian and Laird random-effects model. Subgroup and restricted mean survival time (RMST) analyses were also conducted.
Results: A total of twenty-one studies were included. CI was associated with a 74% higher risk of all-cause mortality (HR: 1.74; 95% CI: 1.48 to 2.04; P < 0.001). Compared to patients without CI, those with CI had significantly lower exercise performance across all parameters: resting heart rate (MD: –6.91 bpm; P < 0.0001), peak heart rate (MD: –34.71 bpm; P < 0.001), heart rate reserve (MD: –28.05 bpm; P < 0.001), exercise duration (MD: –77.68 seconds; P = 0.021), peak workload (MD: –19.15 watts; P < 0.0001), and peak VO2 (MD: –3.31 ml.kg-1.min-1; P < 0.0001). Additionally, VE/VCO2 slope was significantly higher in the CI group (MD: 2.03; P < 0.0001), indicating poorer ventilatory efficiency. Subgroup analysis showed CI was linked to poor survival in both HF patients with reduced and preserved ejection fraction (HR: 1.49 and 2.50, respectively). Additionally, RMST analysis revealed fewer event-free days over five years in patients with CI, with differences of 67 days in the HFrEF subgroup (P < 0.001) and 371 days in the HFpEF subgroup (P < 0.001), compared to their non-CI counterparts.
Conclusion: HF patients with CI have poorer survival and reduced functional and ventilatory efficiency during physical activity. These findings emphasize the importance of this often-overlooked condition in HF patients and suggest that identifying CI and adopting personalized treatment strategies such as exercise rehabilitation and rate-adaptive pacing could potentially improve survival in this high-risk group.
Method: We searched PubMed, Embase, Scopus, and the Cochrane Library for studies published up to April 8, 2025, comparing overall survival and exercise performance in HF patients with and without CI. All-cause mortality was assessed using Cox proportional hazards models based on reconstructed individual patient data. Exercise performance differences were analyzed as mean differences (MD) using the DerSimonian and Laird random-effects model. Subgroup and restricted mean survival time (RMST) analyses were also conducted.
Results: A total of twenty-one studies were included. CI was associated with a 74% higher risk of all-cause mortality (HR: 1.74; 95% CI: 1.48 to 2.04; P < 0.001). Compared to patients without CI, those with CI had significantly lower exercise performance across all parameters: resting heart rate (MD: –6.91 bpm; P < 0.0001), peak heart rate (MD: –34.71 bpm; P < 0.001), heart rate reserve (MD: –28.05 bpm; P < 0.001), exercise duration (MD: –77.68 seconds; P = 0.021), peak workload (MD: –19.15 watts; P < 0.0001), and peak VO2 (MD: –3.31 ml.kg-1.min-1; P < 0.0001). Additionally, VE/VCO2 slope was significantly higher in the CI group (MD: 2.03; P < 0.0001), indicating poorer ventilatory efficiency. Subgroup analysis showed CI was linked to poor survival in both HF patients with reduced and preserved ejection fraction (HR: 1.49 and 2.50, respectively). Additionally, RMST analysis revealed fewer event-free days over five years in patients with CI, with differences of 67 days in the HFrEF subgroup (P < 0.001) and 371 days in the HFpEF subgroup (P < 0.001), compared to their non-CI counterparts.
Conclusion: HF patients with CI have poorer survival and reduced functional and ventilatory efficiency during physical activity. These findings emphasize the importance of this often-overlooked condition in HF patients and suggest that identifying CI and adopting personalized treatment strategies such as exercise rehabilitation and rate-adaptive pacing could potentially improve survival in this high-risk group.
More abstracts on this topic:
5-oxoproline/ OPLAH Axis Alleviates Doxorubicin-induced Cardiomyopathy By Inhibiting Ferroptosis
Jiang Meng, Guo Xinning
β1-adrenergic autoantibodies (β1-AA) augment macropinocytosis in CD4+ T cells, leading to the expansion of CD4+CD28− T cell subsets in heart failure.Sun Fei, Yao Junyan, Li Bingjie, Zhang Suli, Liu Huirong