Final ID: Sa2013
Population Changes in AI Coronary Plaque Volumes over 7 Years
Abstract Body (Do not enter title and authors here): Background: We sought to benchmark long-term changes in coronary artery plaque volumes by creating nomograms from AI-enabled coronary plaque analysis (AI-CPA), derived from a large database of patients with repeat coronary CTA scans.
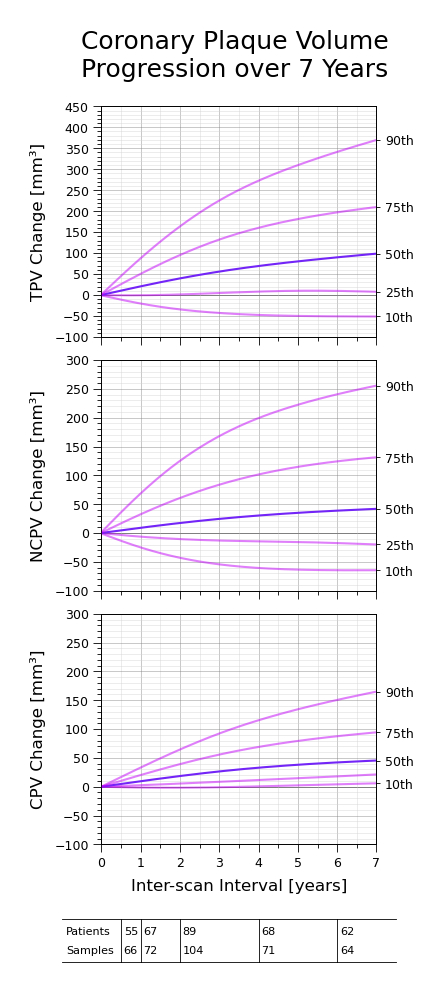
Methods: We analyzed serial coronary CTA images from 342 patients who underwent at least two clinically indicated CTAs (727 CTAs total). Patients with <50 mm3 total plaque volume on baseline scan were excluded. CTAs were acquired between 2006 and 2024 at 64 international sites (93% US) representing diverse CT scanners (GE 60%, Siemens 29%, Philips 6%, Canon 5%) and tube potentials (80-140 kVp, 65% at 120 and 28% at 100 kVp). Total (TPV), calcified (CPV), and non-calcified (NCPV) plaque volumes in vessels >1.8 mm in diameter were quantified using 2nd-generation AI-CPA (Heartflow Inc.). Vessels with significant motion artifacts, stents, or occlusions were excluded. Paired scans were categorized by inter-scan interval based on quintiles (0.5-1, 1-2, 2-4, 4-6, and 6-10 years). PV changes were adjusted for time differences within each interval range, and percentiles (10th, 25th, 50th, 75th, and 90th) calculated. Time-dependent percentiles were smoothed using quadratic splines to construct plaque progression nomograms.
Results: Nomograms were derived from 637 scans of 300 patients (211 male, 60 female, 29 sex unknown), excluding 42 patients with baseline TPV <50 mm3. Median age at baseline scan was 65 (IQR 57-71), female 68, male 63 years. Median baseline findings were TPV 335 (IQR 183–590), NCPV 255 (IQR 142–433), and CPV 68 (IQR 28–153) mm3, with median annualized ΔTPV 18 (IQR -1–50), ΔNCPV 8 (IQR -7–33), and ΔCPV 9 (IQR 2–18) mm3/year. Baseline TPV differed between female and male patients (p<0.001), but no difference was observed in ΔTPV. Baseline TPV was a strong predictor of ΔTPV (p<0.001). Median ΔTPV was not influenced by scanner type or tube potential. Although CPV and median NCPV increased with time, NCPV decreased in 35% of cases, showing the potential of monitoring changes in NCPV and the ratio of NCPV to CPV over time. Treatment information was not available.
Conclusions: We report the first large scale AI-CPA-derived TPV, NCPV, and CPV progression nomograms which can inform future studies of disease progression and modification as well as treatment responses.
Methods: We analyzed serial coronary CTA images from 342 patients who underwent at least two clinically indicated CTAs (727 CTAs total). Patients with <50 mm3 total plaque volume on baseline scan were excluded. CTAs were acquired between 2006 and 2024 at 64 international sites (93% US) representing diverse CT scanners (GE 60%, Siemens 29%, Philips 6%, Canon 5%) and tube potentials (80-140 kVp, 65% at 120 and 28% at 100 kVp). Total (TPV), calcified (CPV), and non-calcified (NCPV) plaque volumes in vessels >1.8 mm in diameter were quantified using 2nd-generation AI-CPA (Heartflow Inc.). Vessels with significant motion artifacts, stents, or occlusions were excluded. Paired scans were categorized by inter-scan interval based on quintiles (0.5-1, 1-2, 2-4, 4-6, and 6-10 years). PV changes were adjusted for time differences within each interval range, and percentiles (10th, 25th, 50th, 75th, and 90th) calculated. Time-dependent percentiles were smoothed using quadratic splines to construct plaque progression nomograms.
Results: Nomograms were derived from 637 scans of 300 patients (211 male, 60 female, 29 sex unknown), excluding 42 patients with baseline TPV <50 mm3. Median age at baseline scan was 65 (IQR 57-71), female 68, male 63 years. Median baseline findings were TPV 335 (IQR 183–590), NCPV 255 (IQR 142–433), and CPV 68 (IQR 28–153) mm3, with median annualized ΔTPV 18 (IQR -1–50), ΔNCPV 8 (IQR -7–33), and ΔCPV 9 (IQR 2–18) mm3/year. Baseline TPV differed between female and male patients (p<0.001), but no difference was observed in ΔTPV. Baseline TPV was a strong predictor of ΔTPV (p<0.001). Median ΔTPV was not influenced by scanner type or tube potential. Although CPV and median NCPV increased with time, NCPV decreased in 35% of cases, showing the potential of monitoring changes in NCPV and the ratio of NCPV to CPV over time. Treatment information was not available.
Conclusions: We report the first large scale AI-CPA-derived TPV, NCPV, and CPV progression nomograms which can inform future studies of disease progression and modification as well as treatment responses.
More abstracts on this topic:
A ChatGLM-based stroke diagnosis and prediction tool
Song Xiaowei, Wang Jiayi, Ma Weizhi, Wu Jian, Wang Yueming, Gao Ceshu, Wei Chenming, Pi Jingtao
A 50% or Greater Reduction in LDL-Cholesterol Is Associated with Improved Long-Term Outcomes and Lower Health Care Utilization After Myocardial Infarction - a SWEDEHEART studyReitan Christian, Watanabe Alexandre, Bash Lori, Galvain Thibaut, Arnet Urs, Jernberg Tomas