Final ID: MP2293
Associations of Predicted CVD risk by the PREVENT Equation with AI-analyzed Coronary Atherosclerotic Plaque Characteristics
Abstract Body (Do not enter title and authors here): Background
The PREVENT equations estimates 10-year total CVD risk using clinical and laboratory data. Its association with coronary plaque morphology using coronary CT angiography (CCTA) remains unclear. Moreover, it is unknown whether lipoprotein(a) [Lp(a)], an established marker of cardiovascular risk, provides additional predictive value for coronary plaque burden beyond that offered by the PREVENT equations.
Objective
Assess the association between predicted 10-year total CVD risk and coronary plaque features, and evaluate whether Lp(a) adds predictive value.
Methods
We conducted a retrospective study, asymptomatic patients without prior cardiovascular events underwent coronary computed tomography angiography (CCTA) between 2018 and 2024. Coronary plaque characteristics were quantified using artificial intelligence (AI)-based analysis. One-way ANOVA was used to assess differences in plaque burden across risk categories using the 10-year total predicted CVD based on the PREVENT equations: low risk (<5%), borderline risk (5-7.4%), intermediate risk (7.5-19.9%), and high risk (≥20%). We used linear regression to assess associations between 10-year total predicted CVD risk and total plaque volume (TPV), calcified plaque (CP), non-calcified plaque (NCP), and low-density non-calcified plaque (LDNCP). Lp(a), modeled per 50 nmol/L, was then added to a model that included 10-year predicted total CVD risk to assess its contribution beyond the PREVENT score.
Results
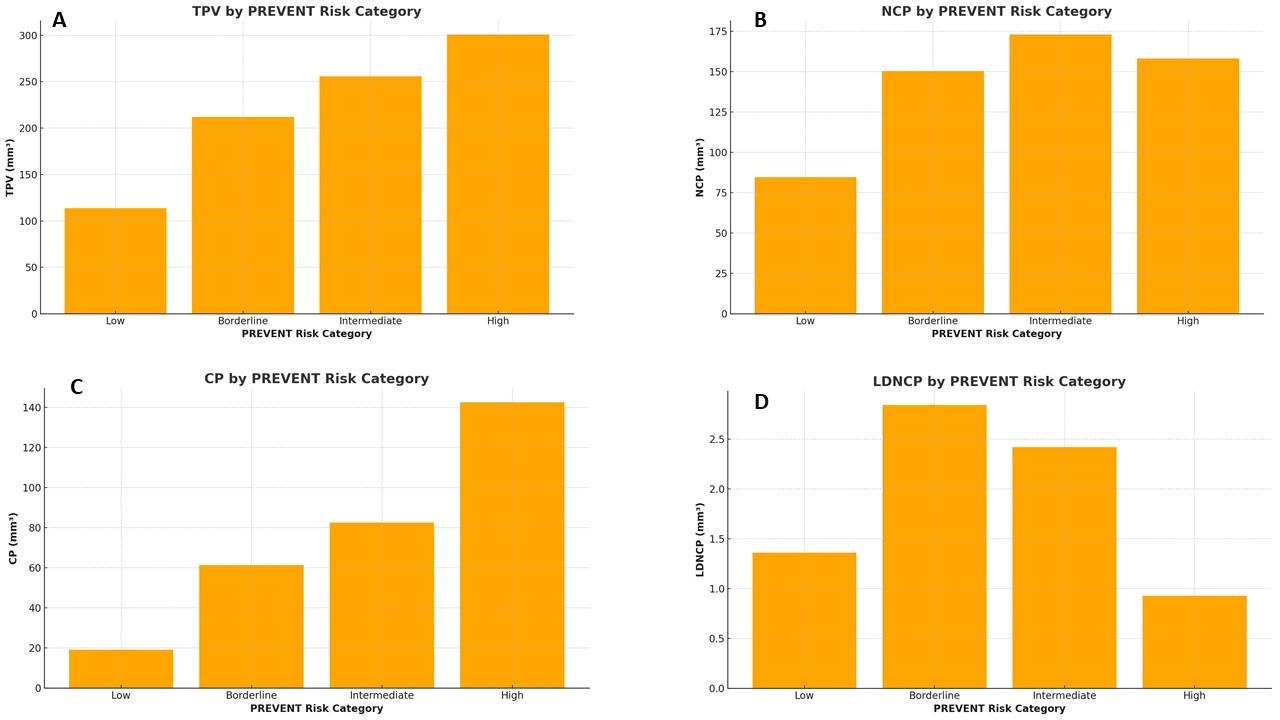
The cohort included 525 adults with a mean age of 55.8 years; 30% were female; and 51% were taking a statin. Total, calcified and non-calcified plaque burden, stenosis severity, and remodeling index increased across higher 10-year total CVD risk categories (p<0.001 for trend; Figure 1). LDNCP was not associated with 10-year total CVD risk. When analyzing the PREVENT score as a continuous variable, higher scores were associated with greater TPV, CP, and NCP (all p<0.001, Table 1), but not LDNCP (p=0.15). Higher Lp(a) was associated with TPV, CP, and NCP after adjustment for 10-year total CVD risk (Table 1).
Conclusion
The 10-year predicted total CVD risk estimated by the PREVENT equations was associated with coronary plaque burden, including calcified and non-calcified components. These results support estimating 10-year predicted total CVD risk using the PREVENT equations as a tool for subclinical atherosclerosis risk assessment and highlight the relevance of Lp(a) in identifying residual plaque risk.
The PREVENT equations estimates 10-year total CVD risk using clinical and laboratory data. Its association with coronary plaque morphology using coronary CT angiography (CCTA) remains unclear. Moreover, it is unknown whether lipoprotein(a) [Lp(a)], an established marker of cardiovascular risk, provides additional predictive value for coronary plaque burden beyond that offered by the PREVENT equations.
Objective
Assess the association between predicted 10-year total CVD risk and coronary plaque features, and evaluate whether Lp(a) adds predictive value.
Methods
We conducted a retrospective study, asymptomatic patients without prior cardiovascular events underwent coronary computed tomography angiography (CCTA) between 2018 and 2024. Coronary plaque characteristics were quantified using artificial intelligence (AI)-based analysis. One-way ANOVA was used to assess differences in plaque burden across risk categories using the 10-year total predicted CVD based on the PREVENT equations: low risk (<5%), borderline risk (5-7.4%), intermediate risk (7.5-19.9%), and high risk (≥20%). We used linear regression to assess associations between 10-year total predicted CVD risk and total plaque volume (TPV), calcified plaque (CP), non-calcified plaque (NCP), and low-density non-calcified plaque (LDNCP). Lp(a), modeled per 50 nmol/L, was then added to a model that included 10-year predicted total CVD risk to assess its contribution beyond the PREVENT score.
Results
The cohort included 525 adults with a mean age of 55.8 years; 30% were female; and 51% were taking a statin. Total, calcified and non-calcified plaque burden, stenosis severity, and remodeling index increased across higher 10-year total CVD risk categories (p<0.001 for trend; Figure 1). LDNCP was not associated with 10-year total CVD risk. When analyzing the PREVENT score as a continuous variable, higher scores were associated with greater TPV, CP, and NCP (all p<0.001, Table 1), but not LDNCP (p=0.15). Higher Lp(a) was associated with TPV, CP, and NCP after adjustment for 10-year total CVD risk (Table 1).
Conclusion
The 10-year predicted total CVD risk estimated by the PREVENT equations was associated with coronary plaque burden, including calcified and non-calcified components. These results support estimating 10-year predicted total CVD risk using the PREVENT equations as a tool for subclinical atherosclerosis risk assessment and highlight the relevance of Lp(a) in identifying residual plaque risk.
More abstracts on this topic:
A Multimodal Artificial Intelligence Signature of Advanced Cardiac and Vascular Aging Defines Elevated Risk of Cardiovascular Disease
Perera Sudheesha, Biswas Dhruva, Dhingra Lovedeep, Aminorroaya Arya, Coppi Andreas, Khera Rohan
AI-enabled Plaque Phenotype Analysis of Coronary Computed Tomography Angiography Findings in Patients with Nonacute Chest Pain using FFRCT: Results from the PRECISE TrialJukema Ruurt, Chow Benjamin, Kelsey Michelle, Nanna Michael, Vemulapalli Sreekanth, Mark Daniel, Leipsic Jonathon, Douglas Pamela, Ferencik Maros, Curzen Nick, Weir-mccall Jonathan, Stone Gregg, Rogers Campbell, Mullen Sarah, Ng Nicholas