Final ID: Sa2037
Cardiorenal Protective Effects of Anti-diabetic Drugs in Early Stage Cardiovascular-Kidney-Metabolic Syndrome: A Multicenter, Time-Varying Analysis
Abstract Body (Do not enter title and authors here): Introduction: There is a lack of direct real-world comparisons of specific anti-diabetic agents (ADAs) concerning their cardiovascular and renal effects in the early stages of Cardiovascular-kidney-metabolic (CKM) syndrome.
Research Questions: To evaluate the distinct effects associated with various ADAs among patients in early CKM stage.
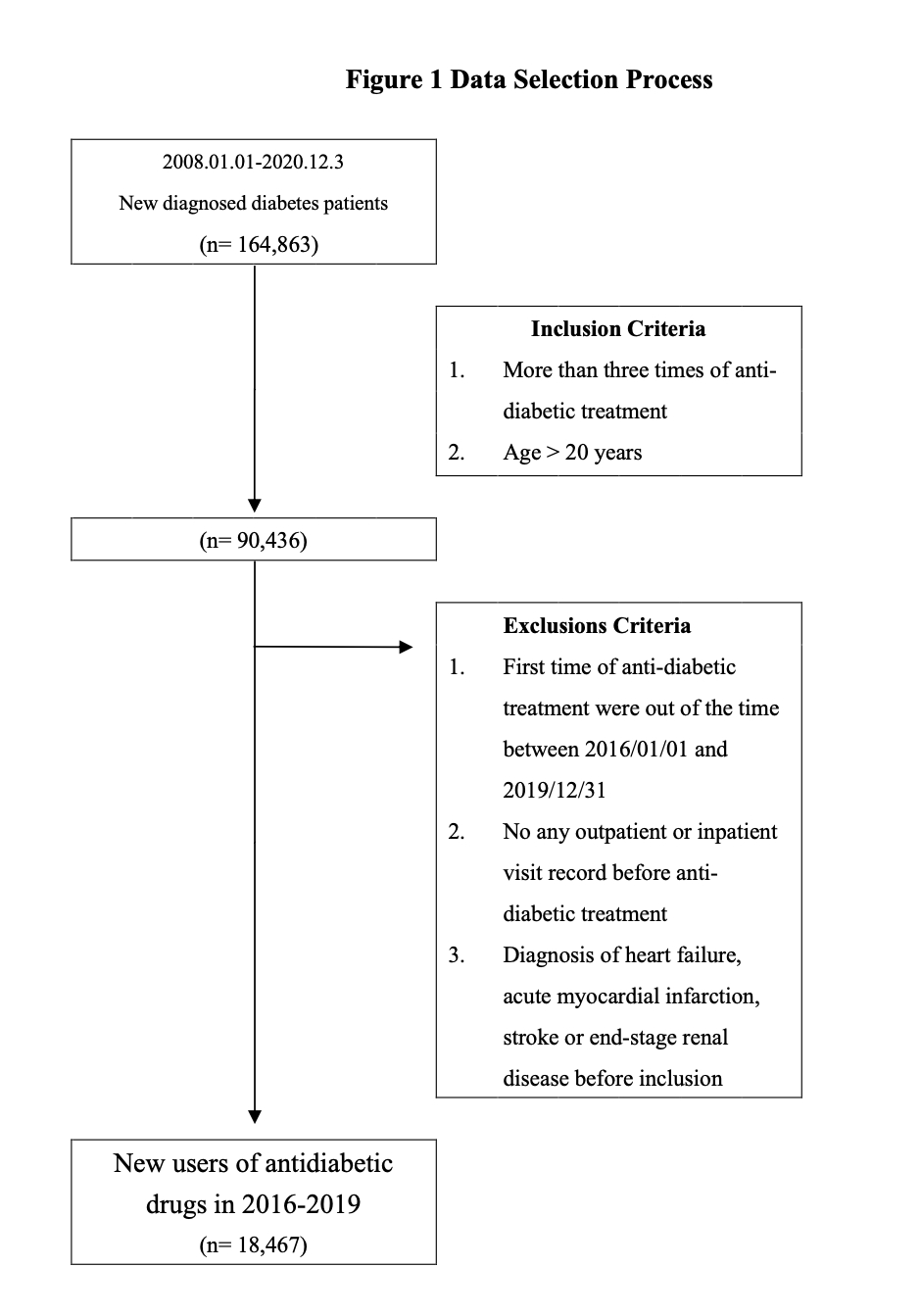
Methods: Between 2016 and 2019, a total of 18,467 patients with newly diagnosis of diabetes were retrospectively enrolled from Taipei Medical University Clinical Research Database. The modeling of time-varying exposure for eight prevalent classes of ADAs (SGLT2 inhibitors, metformin, sulfonylureas, thiazolidinediones, alpha-glucosidase inhibitors, meglitinides, DPP-4 inhibitors, and insulin) was conducted to examine their associations with cardiovascular disease, all-cause mortality, and end-stage renal disease (ESRD).
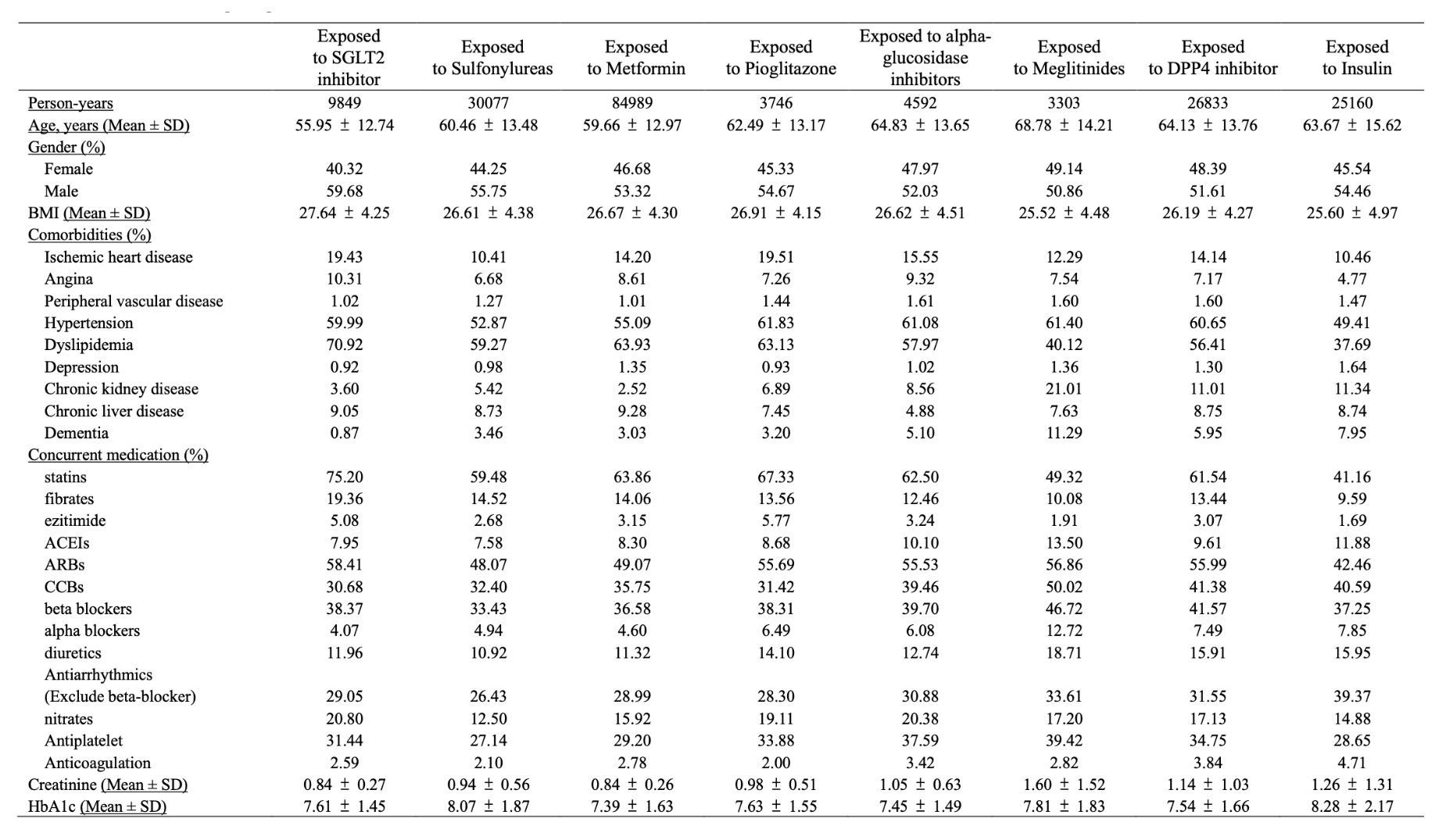
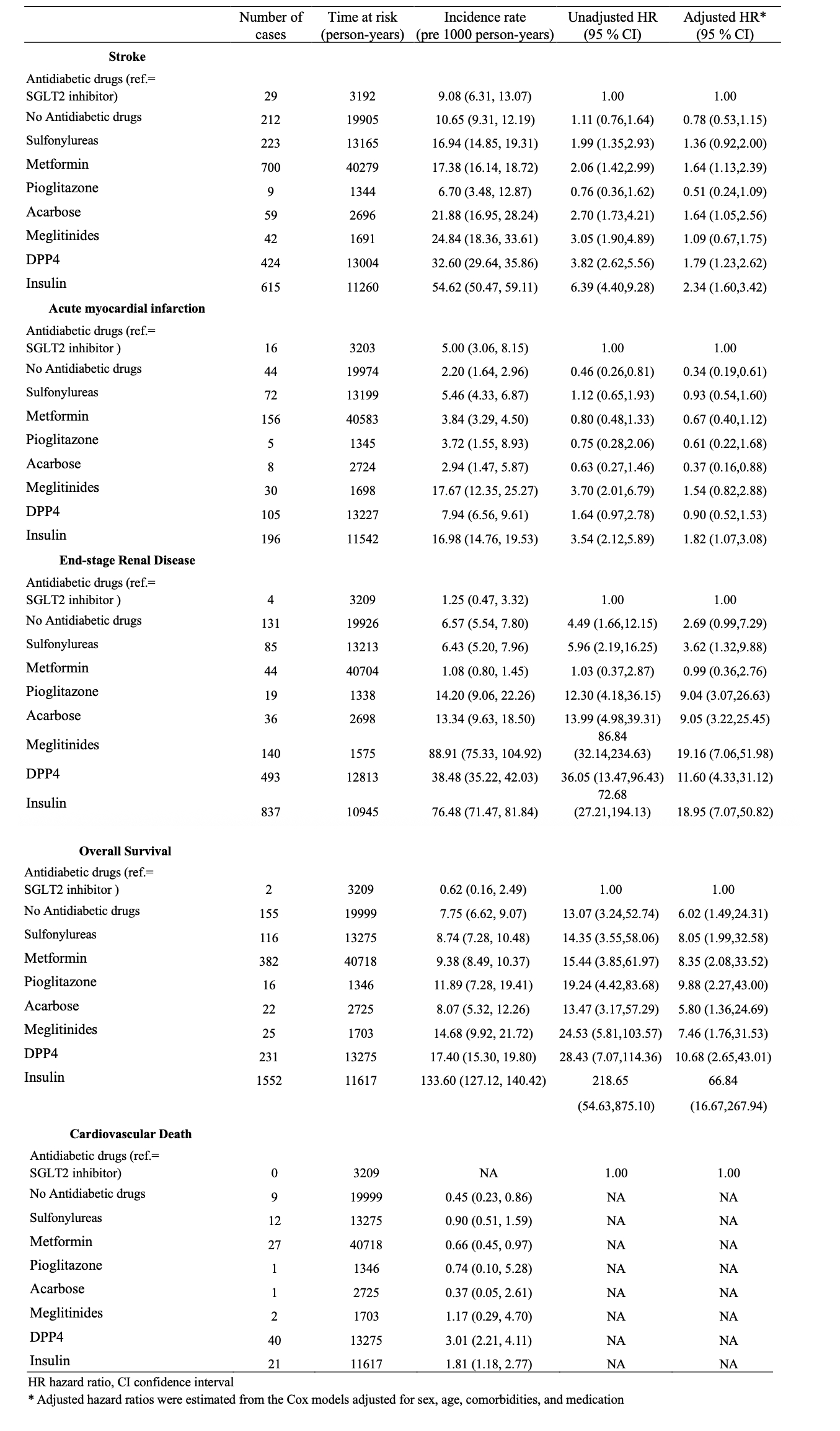
Results: In this cohort, the mean age across the drug groups ranged from 56 to 69 years, with approximately 9% having chronic kidney disease and an average BMI of 26 kg/m^2 in all groups. In a comparative analysis with non-users, most ADAs showed a significant reduction in the risks associated with cardiovascular diseases, including stroke and acute myocardial infarction (AMI), after adjusting for sex, age, comorbidities, and concurrent medication use. Notably, insulin exhibited contrary findings, indicating an elevated risk, with an adjusted hazard ratio (aHR) of 1.65 (95% confidence interval [CI]: 1.49-1.83) for stroke, and aHR of 3.00 (95% CI: 2.70-3.33) for AMI. Furthermore, all ADAs, with the exception of insulin, have been associated with a reduction in all-cause mortality (aHR: 8.26, 95% CI 7.55-9.04). Compared to SGLT2i, all ADAs show a significantly higher risk of developing ESRD and all-cause mortality, with an adjusted hazard ratio ranging from 3.62 to 19.16 and 5.80 to 66.84, respectively. Non-SGLT2i regimens increased stroke risk in men and amplified ESRD, particularly in patients <65 years or BMI ≥ 27 kg/m^2; absence of SGLT2i therapy raised all-cause mortality most in men, the elderly, and less-obese individuals.
Conclusions: In early-stage CKM, most ADAs lessen cardiovascular risk, but SGLT2i uniquely deliver superior renoprotection and survival advantages. Their benefits are most pronounced in younger, obese and male subgroups, suggesting SGLT2i should be prioritized early in the CKM trajectory, while insulin therapy warrants careful risk–benefit reassessment.
Research Questions: To evaluate the distinct effects associated with various ADAs among patients in early CKM stage.
Methods: Between 2016 and 2019, a total of 18,467 patients with newly diagnosis of diabetes were retrospectively enrolled from Taipei Medical University Clinical Research Database. The modeling of time-varying exposure for eight prevalent classes of ADAs (SGLT2 inhibitors, metformin, sulfonylureas, thiazolidinediones, alpha-glucosidase inhibitors, meglitinides, DPP-4 inhibitors, and insulin) was conducted to examine their associations with cardiovascular disease, all-cause mortality, and end-stage renal disease (ESRD).
Results: In this cohort, the mean age across the drug groups ranged from 56 to 69 years, with approximately 9% having chronic kidney disease and an average BMI of 26 kg/m^2 in all groups. In a comparative analysis with non-users, most ADAs showed a significant reduction in the risks associated with cardiovascular diseases, including stroke and acute myocardial infarction (AMI), after adjusting for sex, age, comorbidities, and concurrent medication use. Notably, insulin exhibited contrary findings, indicating an elevated risk, with an adjusted hazard ratio (aHR) of 1.65 (95% confidence interval [CI]: 1.49-1.83) for stroke, and aHR of 3.00 (95% CI: 2.70-3.33) for AMI. Furthermore, all ADAs, with the exception of insulin, have been associated with a reduction in all-cause mortality (aHR: 8.26, 95% CI 7.55-9.04). Compared to SGLT2i, all ADAs show a significantly higher risk of developing ESRD and all-cause mortality, with an adjusted hazard ratio ranging from 3.62 to 19.16 and 5.80 to 66.84, respectively. Non-SGLT2i regimens increased stroke risk in men and amplified ESRD, particularly in patients <65 years or BMI ≥ 27 kg/m^2; absence of SGLT2i therapy raised all-cause mortality most in men, the elderly, and less-obese individuals.
Conclusions: In early-stage CKM, most ADAs lessen cardiovascular risk, but SGLT2i uniquely deliver superior renoprotection and survival advantages. Their benefits are most pronounced in younger, obese and male subgroups, suggesting SGLT2i should be prioritized early in the CKM trajectory, while insulin therapy warrants careful risk–benefit reassessment.
More abstracts on this topic:
Associations between circulating reproductive hormones and cardiovascular-kidney-metabolic syndrome in older men
Hsu Benjumin
Cardiorenal Interaction Assessment via ECG Features: A Study using Dynamic Time Warping and Extracted Feature ClusteringZhao Sally, Adhin Bhavna, Zhan Ye, Fisch Sudeshna