Final ID: MP278
Early Partial ECMO Flow Is Associated With Higher Survival in Patients With Cardiogenic Shock With Reduced and Preserved Systemic Pulse Pressure: An ELSO Registry Analysis
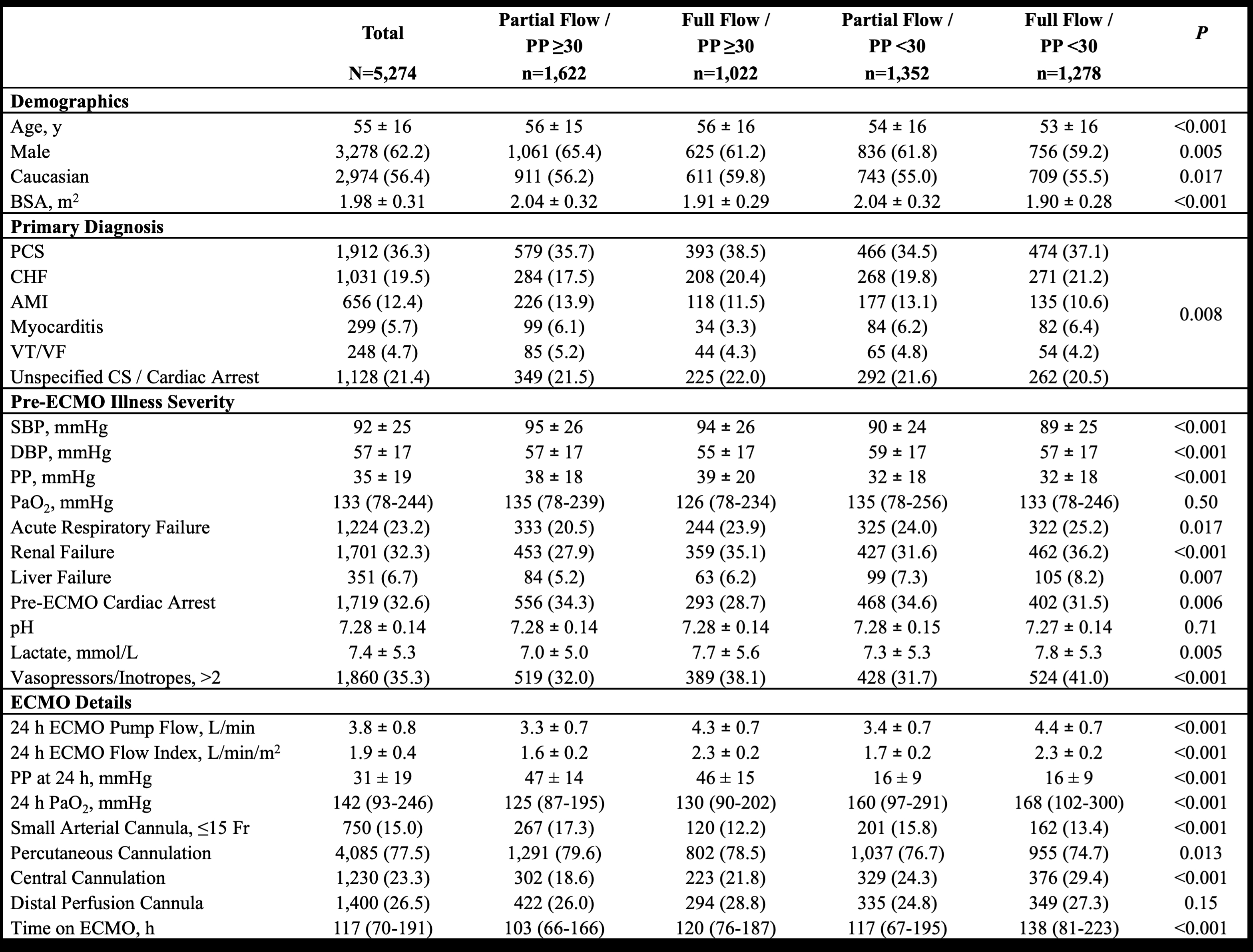
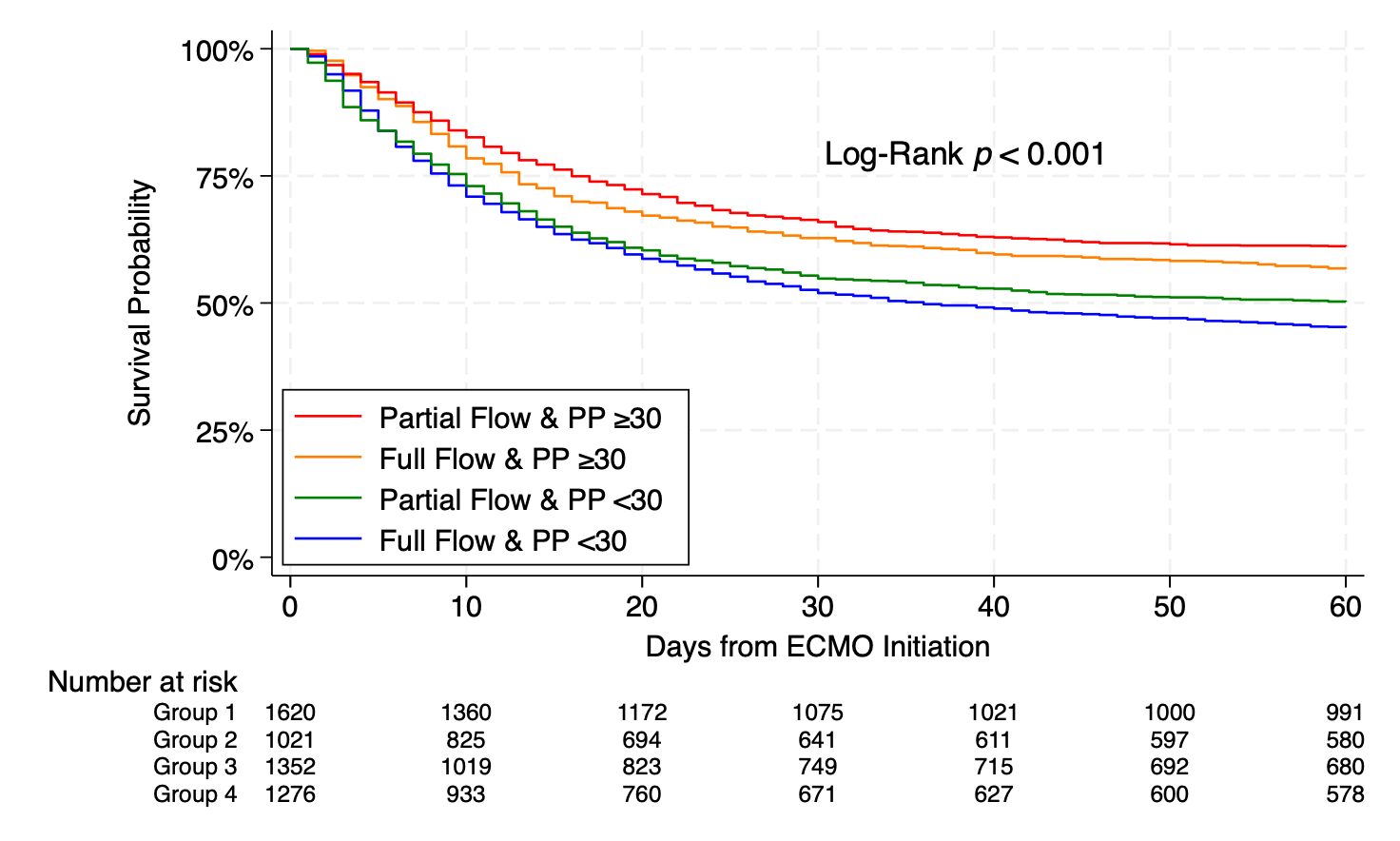
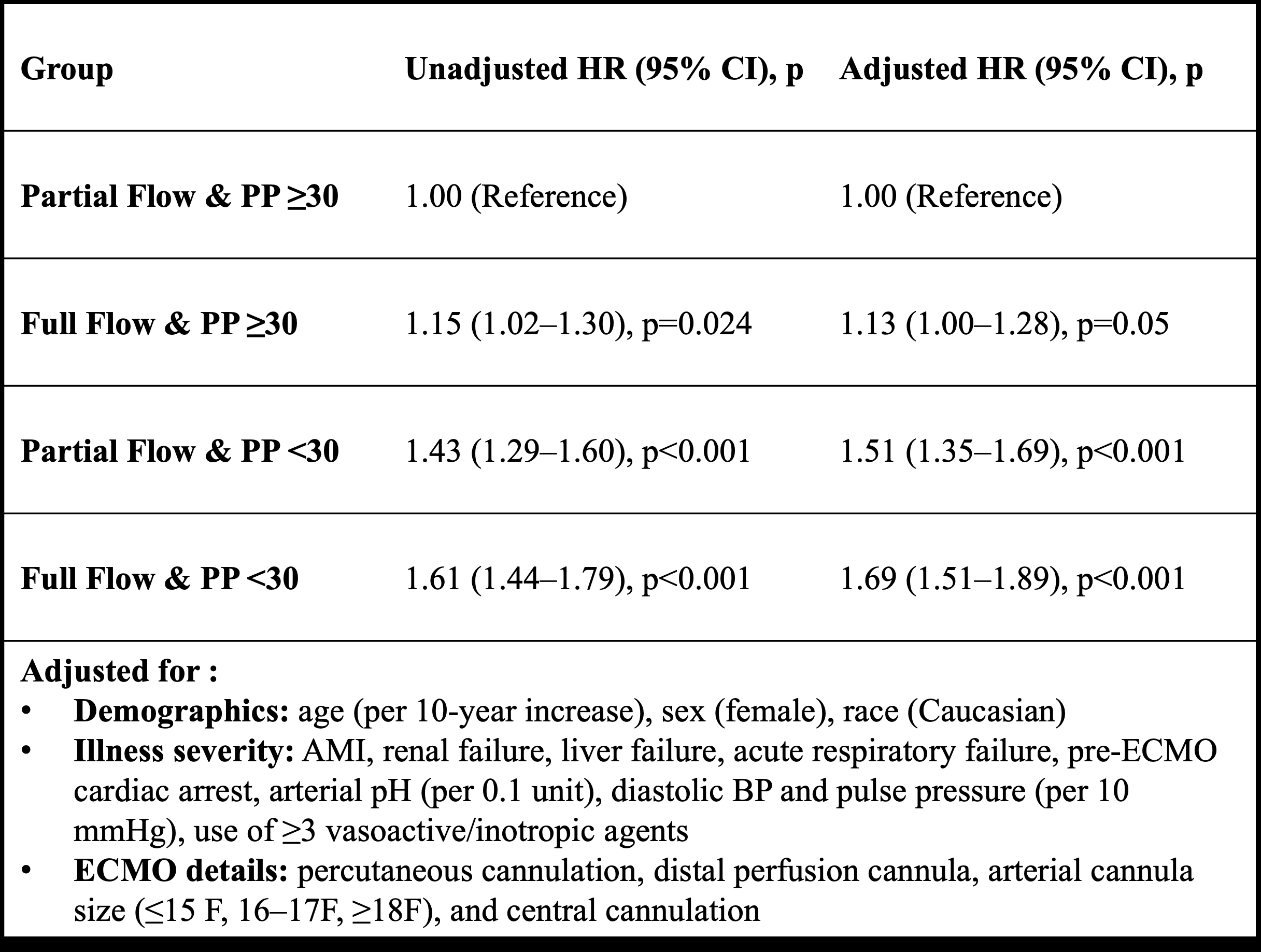
Abstract Body (Do not enter title and authors here): Introduction: In cardiogenic shock (CS) patients supported with venoarterial extracorporeal membrane oxygenation (VA-ECMO), emerging observational evidence suggests potential benefit from the use of a partial ECMO flow strategy, but whether these findings extend across a spectrum of residual native heart function is unknown. Systemic pulse pressure (PP) is a reasonable surrogate of native heart function during ECMO support, and the interaction between early ECMO flow and PP is not well understood. Hypothesis: CS patients receiving VA-ECMO with early partial versus full ECMO flow will have higher inpatient survival across both reduced and preserved PP at 24 hours of support. Methods: We queried the ELSO Registry (2018–2023) for adults with CS supported with VA-ECMO, excluding patients with ECPR or with a concomitant left ventricular mechanical unloading device. At 24 hours of support, patients were stratified into four groups based on ECMO flow index (partial <2.0 vs full ≥2.0 L/min/m2 flow) and PP (reduced < 30mmHg versus preserved ≥30 mmHg). The primary outcome of 60-day in-hospital survival was compared using Kaplan-Meier time-to-event analysis and multivariable Cox proportional hazards modeling. Results: Among 5,274 CS patients receiving VA-ECMO, 50% had preserved pulse pressure and 56% received partial flow at 24 hours. Patients with preserved PP receiving partial flow had markers of lower baseline illness severity compared to the other groups (Table 1). Patients with preserved PP and partial flow had the highest 60-day survival at 61%, while those with reduced PP and full flow had the lowest survival at 45% (log-rank p<0.001) (Figure 1). This relationship between flow index and PP groups with survival persisted in multivariable Cox modeling (Table 2). Partial flow was associated with significantly higher inpatient survival in both PP groups: 61% vs 57% in patients with PP ≥30 mmHg (log-rank p=0.021) and 50% vs 45% in patients with PP <30 mmHg (log-rank p=0.033). Conclusions: Among adults with CS supported on VA-ECMO, the use of partial versus full ECMO flow at 24 hours was associated with higher 60-day in-hospital survival in patients with both reduced and preserved systemic pulse pressure, suggesting potential benefit of a partial flow strategy across a spectrum of residual native heart function.
More abstracts on this topic:
A recombinant protein oxygen carrier with reduced nitric oxide scavenging as a blood substitute for resuscitation
Xu Qinzi, Rochon Elizabeth, Bocian Kaitlin, Huang Xue, Poropatich Ronald, Gladwin Mark, Tejero Jesus, Rose Jason, Rodriguez Deborah, Hwang Hyon, Turner Bryan, Hunt Thomas, Dent Matthew, Demartino Anthony, Abdelghany Youmna, Chen Xiukai
Admission Cell-free DNA Predicts Cardiogenic Shock Progression and In-Hospital MortalityPark Ashley, Kong Hyesik, Andargie Temesgen, Jang Moon, Solomon Michael, Brusca Samuel, Barnett Christopher, Obrien Connor, Agbor-enoh Sean