Final ID: MP627
Contemporary Trends and Disparities in Premature Ischemic Stroke-Related Mortality in the United States, 1999–2022
Abstract Body (Do not enter title and authors here): Background:
Ischemic stroke, responsible for 87% of all strokes in the U.S., is a major cause of death and disability. Premature mortality from ischemic stroke, defined as death before age 65, leads to significant life year losses. However, national trends and disparities in premature ischemic stroke mortality remain unexplored.
Aims:
To evaluate national, demographic, and regional trends in premature ischemic stroke-related mortality in the U.S. from 1999 to 2022.
Methods:
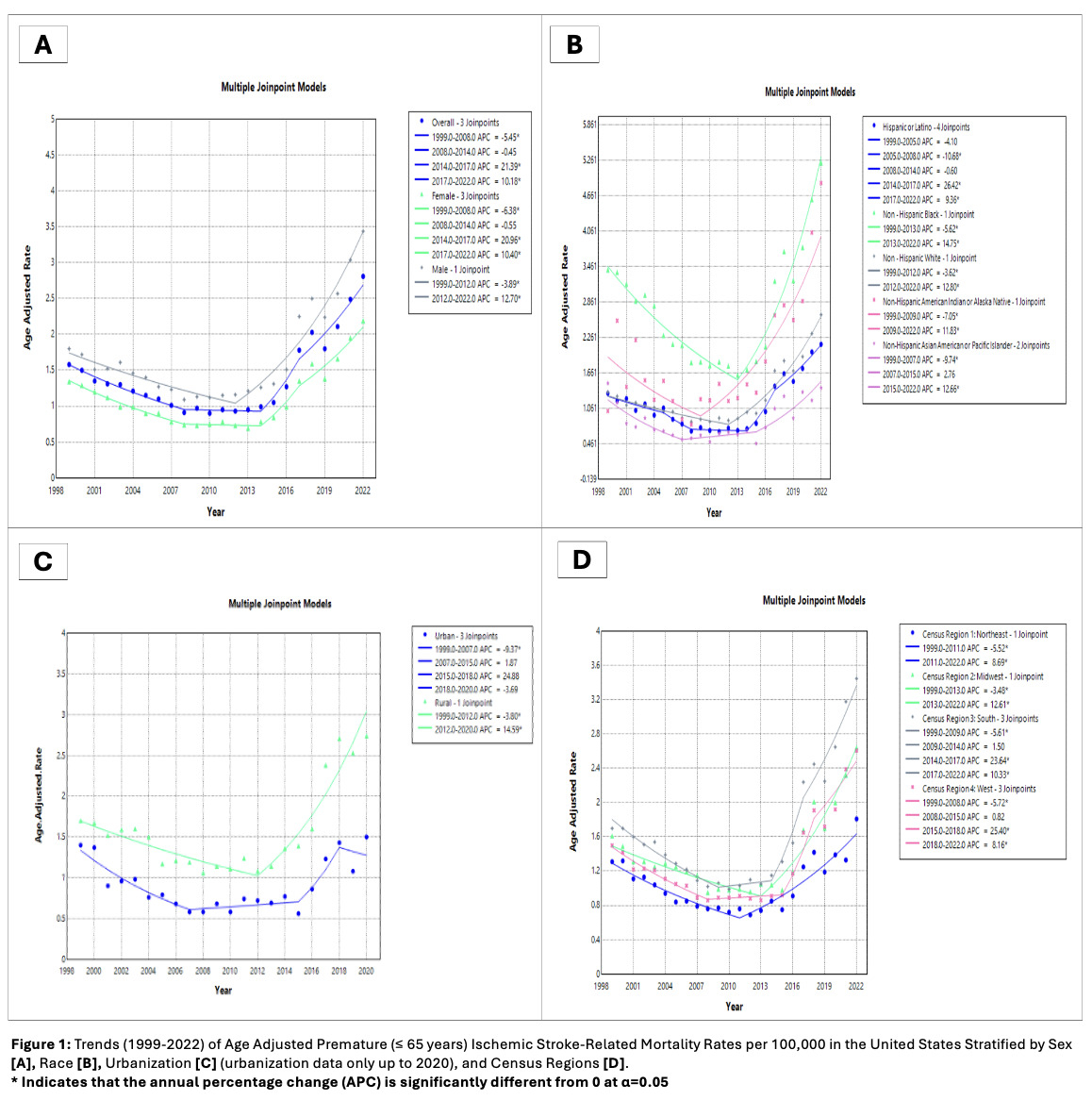
CDC WONDER data were used to identify deaths in individuals ≤ 65 years of age where ischemic stroke (ICD-10: I63) was listed either as an underlying or contributing cause. Age-adjusted mortality rates (AAMRs) per 100,000 and annual percent changes (APCs) with 95% confidence intervals (CIs) were estimated using Joinpoint regression. Analyses were stratified by sex, race/ethnicity, urbanization, and U.S. Census region.
Results:
From 1999 to 2022, 78,816 premature ischemic stroke-related deaths occurred in the US. Overall AAMRs declined from 1.58 in 1999 to 0.91 in 2008 (APC: –5.45), slowed through 2014 (APC: –0.45), then rose sharply to 1.78 in 2017 (APC: +21.39) and 2.81 in 2022 (APC: +10.18). Males had consistently higher mortality than females, with AAMRs rising from 1.80 in 1999 to 3.44 in 2022, compared to an increase from 1.34 to 2.19 in females over the same period. In 2022, non-Hispanic (NH) Black adults had the highest AAMR (5.21; APC: +14.75 [2013–2022]), followed by NH American Indian or Alaska Native (4.87), NH White (2.64), Hispanic or Latino (2.14), and NH Asian American or Pacific Islander (1.40). Rural AAMRs remained consistently higher than urban rates, with AAMRs declining from 1.70 in 1999 to 1.06 in 2012 (APC: –3.80%), then rising to 2.38 in 2020 (APC: +14.59%). Urban rates dropped from 1.40 to 0.58 by 2007 (APC: –9.37%), rose to 1.23 by 2018 (APC: +24.88%), and had a non-significant slight decline through 2020. The South consistently had the highest AAMRs across all regions, reaching 3.45 in 2022, followed by the Midwest (2.64), West (2.61), and Northeast (1.81).
Conclusion:
Premature ischemic stroke mortality in the U.S. has sharply reversed since the mid-2010s, with the greatest increases among males, NH Black individuals, rural populations, and the South. Given the substantial years of life lost associated with premature ischemic stroke-related mortality, these trends underscore widening disparities and the need for urgent, equity-focused prevention, treatment, and care.
Ischemic stroke, responsible for 87% of all strokes in the U.S., is a major cause of death and disability. Premature mortality from ischemic stroke, defined as death before age 65, leads to significant life year losses. However, national trends and disparities in premature ischemic stroke mortality remain unexplored.
Aims:
To evaluate national, demographic, and regional trends in premature ischemic stroke-related mortality in the U.S. from 1999 to 2022.
Methods:
CDC WONDER data were used to identify deaths in individuals ≤ 65 years of age where ischemic stroke (ICD-10: I63) was listed either as an underlying or contributing cause. Age-adjusted mortality rates (AAMRs) per 100,000 and annual percent changes (APCs) with 95% confidence intervals (CIs) were estimated using Joinpoint regression. Analyses were stratified by sex, race/ethnicity, urbanization, and U.S. Census region.
Results:
From 1999 to 2022, 78,816 premature ischemic stroke-related deaths occurred in the US. Overall AAMRs declined from 1.58 in 1999 to 0.91 in 2008 (APC: –5.45), slowed through 2014 (APC: –0.45), then rose sharply to 1.78 in 2017 (APC: +21.39) and 2.81 in 2022 (APC: +10.18). Males had consistently higher mortality than females, with AAMRs rising from 1.80 in 1999 to 3.44 in 2022, compared to an increase from 1.34 to 2.19 in females over the same period. In 2022, non-Hispanic (NH) Black adults had the highest AAMR (5.21; APC: +14.75 [2013–2022]), followed by NH American Indian or Alaska Native (4.87), NH White (2.64), Hispanic or Latino (2.14), and NH Asian American or Pacific Islander (1.40). Rural AAMRs remained consistently higher than urban rates, with AAMRs declining from 1.70 in 1999 to 1.06 in 2012 (APC: –3.80%), then rising to 2.38 in 2020 (APC: +14.59%). Urban rates dropped from 1.40 to 0.58 by 2007 (APC: –9.37%), rose to 1.23 by 2018 (APC: +24.88%), and had a non-significant slight decline through 2020. The South consistently had the highest AAMRs across all regions, reaching 3.45 in 2022, followed by the Midwest (2.64), West (2.61), and Northeast (1.81).
Conclusion:
Premature ischemic stroke mortality in the U.S. has sharply reversed since the mid-2010s, with the greatest increases among males, NH Black individuals, rural populations, and the South. Given the substantial years of life lost associated with premature ischemic stroke-related mortality, these trends underscore widening disparities and the need for urgent, equity-focused prevention, treatment, and care.
More abstracts on this topic:
A Measurement Model of Socioeconomic Status and its Association with Cardiovascular Disease in the Hispanic Community Health Study/Study of Latinos
Cordero Christina, Llabre Maria, Romaker Emma, Kobayashi Marissa, Gianola Morgan, Gallo Linda, Isasi Carmen, Perreira Krista, Corsino Leonor, Zhou Laura
A Meta-Analysis of Prospective Studies Comparing Short and Longterm Outcomes of Trans-Catheter Aortic Valve Replacement in Patient with and without Cancer:Khan Muhammad Aslam, Haider Adnan, Haider Taimoor, Bhattarai Shraddha, Khan Bilal, Lamichhane Bikal, Shafique Nouman, Rahman Hammad, Aafreen Asna, Muhammad Anza, Bhatia Hitesh, Khan Abid Nawaz Khan, Akbar Usman, Khan Alamzaib