Final ID: MP573
Geographic and Demographic Trends in Aortic Aneurysm and Dissection Mortality Among U.S. Adults Aged 65–75, 1999–2020
Abstract Body (Do not enter title and authors here): Background:
Aortic aneurysm and dissection (AAD) are highly fatal in older adults. While AAD mortality has declined since 1999, reductions have been uneven across U.S. regions, sexes, and racial/ethnic groups, likely due to healthcare variability.
Methods:
We used CDC WONDER data (1999–2020) to identify AAD deaths among adults aged 65–75. We focused on this group because AAD incidence peaks here, Medicare coverage ensures near-complete reporting, and guideline-based screening is recommended—maximizing data quality and translational value. After excluding 577 unreliable records, 55,531 deaths remained. Crude mortality rates per 100,000 were calculated by sex and race/ethnicity (White, Black, Asian or Pacific Islander [API], American Indian or Alaska Native [AIAN]) using census denominators. State trends were assessed versus vascular surgeon density, Medicaid expansion, rural hospital closures, smoking, and hypertension.
Results:
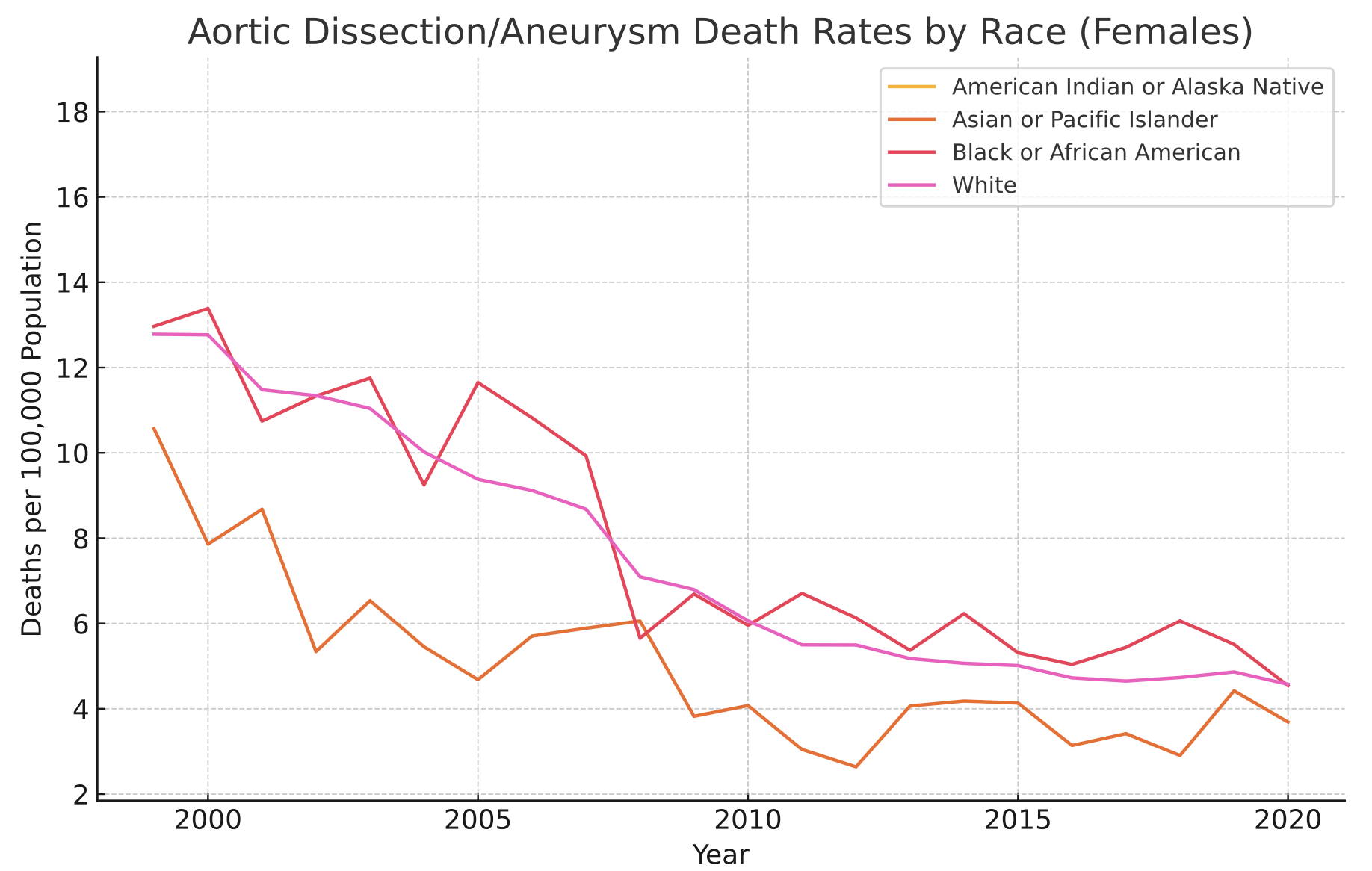
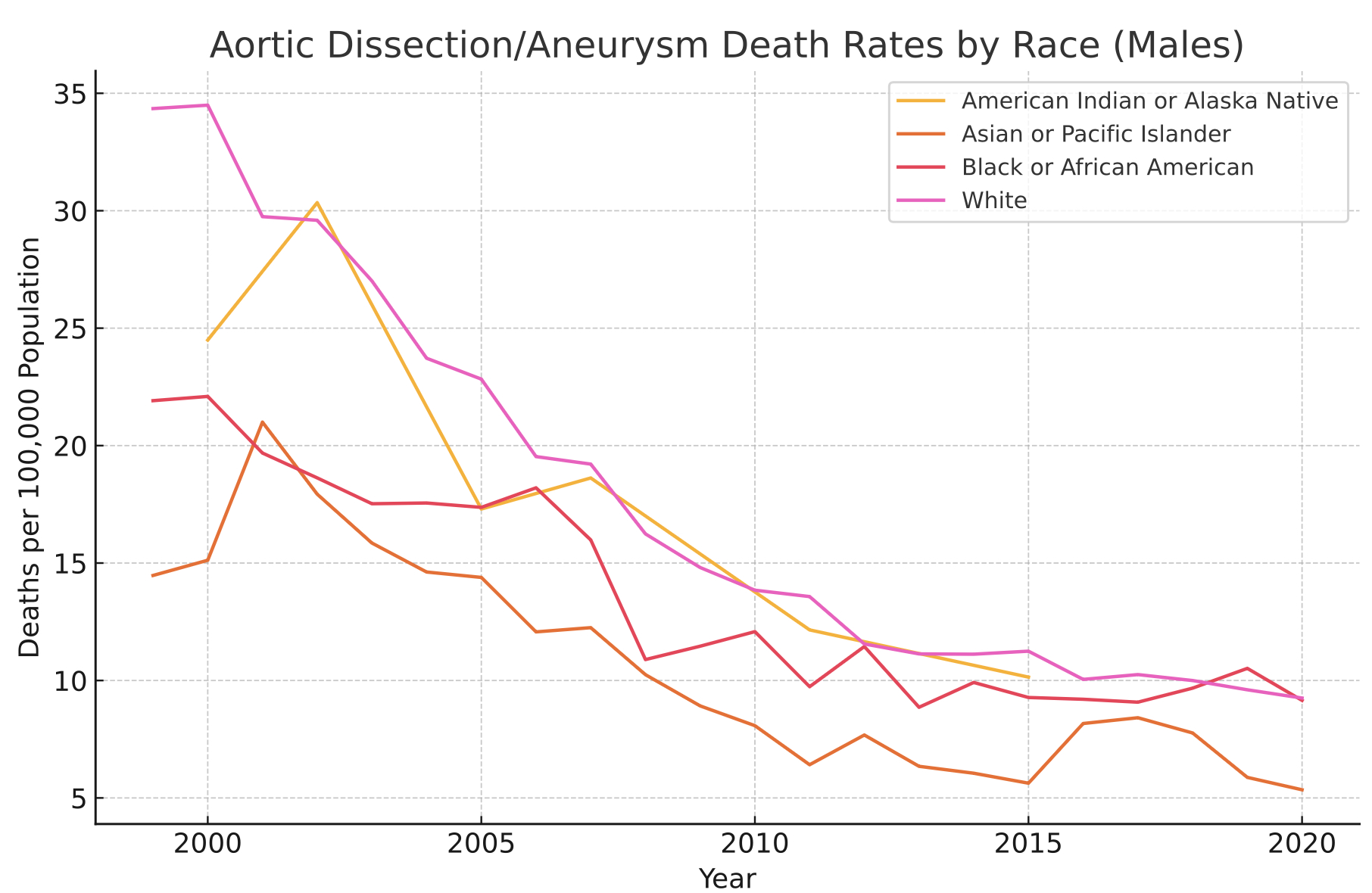
From 1999 to 2020, there were 36,791 AAD deaths among males and 18,740 among females. Male mortality declined from 32.7 to 9.0 (–72.4%); female from 12.7 to 4.5 (–64.5%). Males showed higher rates and volatility, with spikes in 2000, 2015, and 2017. Average annual decline was larger for males (–1.1) than females (–0.39), peaking in 2008. Black females had slightly greater mean declines (–0.40) than White females (–0.39); White males declined more than Black males (–1.1 vs. –0.6). API adults improved steadily (females: 10.6 to 3.7; males: 14.5 to 5.3). AIAN data were too sparse for reliable conclusions.
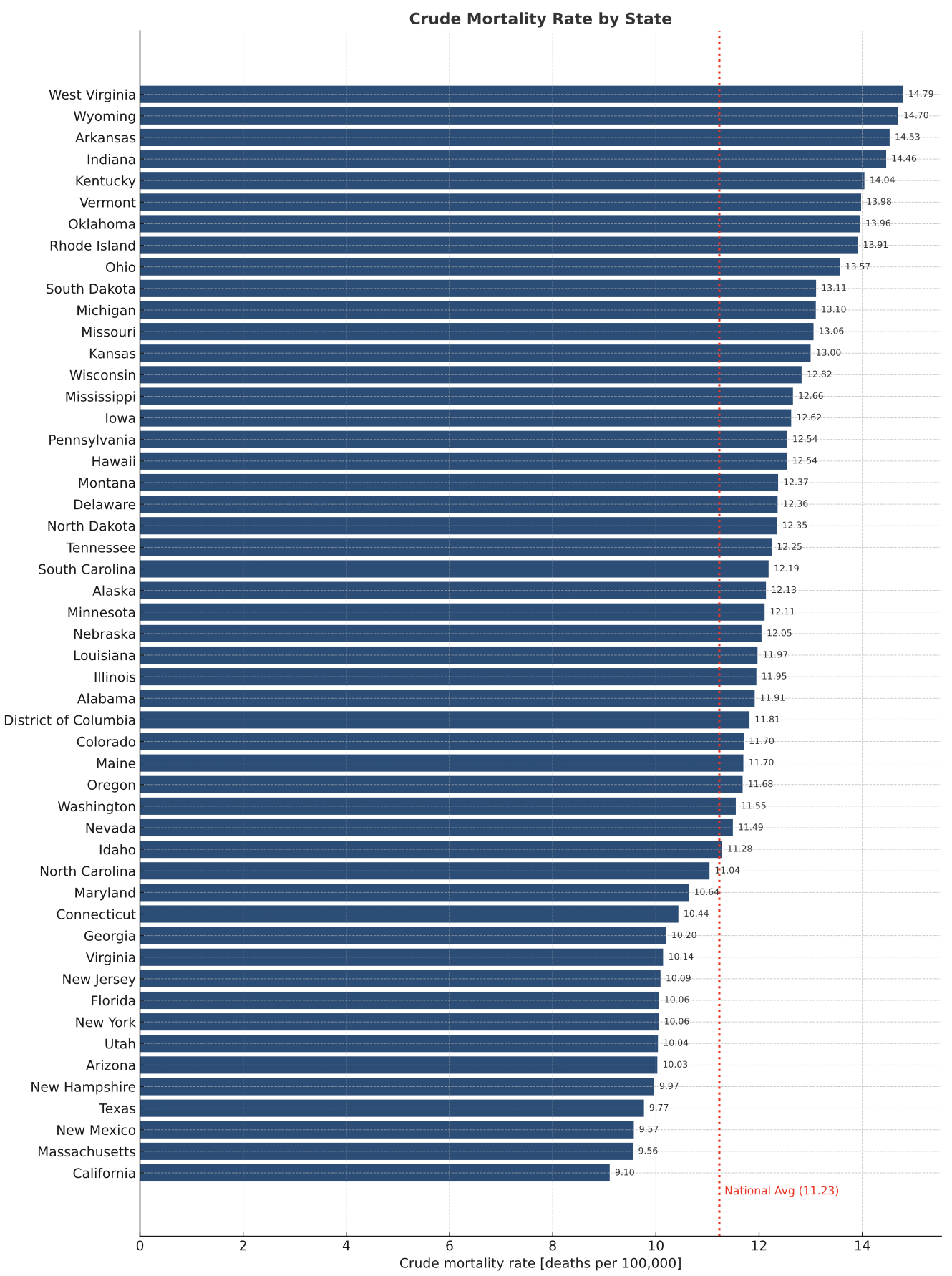
High-mortality states included West Virginia (14.8), Wyoming (14.7), Arkansas (14.5), and Indiana (14.4), clustered in Appalachia and rural Midwest/South. Low-mortality states—California (5.6), Massachusetts (6.0), and New York (6.2)—had stronger healthcare systems. High-burden states had under 0.8 vascular surgeons per 100,000 vs. ≥1.5 in low-burden states. Uninsured rates exceeded 12% vs. under 6%. Medicaid expansion was delayed. Since 2005, 193 rural hospitals have closed. Smoking rates were 21% vs. 10%; uncontrolled hypertension 30% vs. 18%.
Conclusions:
From 1999 to 2020, AAD mortality declined substantially but unevenly across sex, race, and geography. Disparities reflect access, coverage, and prevention gaps. Addressing these requires specialty expansion, rural hospital support, earlier Medicaid uptake, and community prevention.
Keywords: Aortic aneurysm; Aortic dissection; Mortality trends; Racial disparities; Geographic variation
Aortic aneurysm and dissection (AAD) are highly fatal in older adults. While AAD mortality has declined since 1999, reductions have been uneven across U.S. regions, sexes, and racial/ethnic groups, likely due to healthcare variability.
Methods:
We used CDC WONDER data (1999–2020) to identify AAD deaths among adults aged 65–75. We focused on this group because AAD incidence peaks here, Medicare coverage ensures near-complete reporting, and guideline-based screening is recommended—maximizing data quality and translational value. After excluding 577 unreliable records, 55,531 deaths remained. Crude mortality rates per 100,000 were calculated by sex and race/ethnicity (White, Black, Asian or Pacific Islander [API], American Indian or Alaska Native [AIAN]) using census denominators. State trends were assessed versus vascular surgeon density, Medicaid expansion, rural hospital closures, smoking, and hypertension.
Results:
From 1999 to 2020, there were 36,791 AAD deaths among males and 18,740 among females. Male mortality declined from 32.7 to 9.0 (–72.4%); female from 12.7 to 4.5 (–64.5%). Males showed higher rates and volatility, with spikes in 2000, 2015, and 2017. Average annual decline was larger for males (–1.1) than females (–0.39), peaking in 2008. Black females had slightly greater mean declines (–0.40) than White females (–0.39); White males declined more than Black males (–1.1 vs. –0.6). API adults improved steadily (females: 10.6 to 3.7; males: 14.5 to 5.3). AIAN data were too sparse for reliable conclusions.
High-mortality states included West Virginia (14.8), Wyoming (14.7), Arkansas (14.5), and Indiana (14.4), clustered in Appalachia and rural Midwest/South. Low-mortality states—California (5.6), Massachusetts (6.0), and New York (6.2)—had stronger healthcare systems. High-burden states had under 0.8 vascular surgeons per 100,000 vs. ≥1.5 in low-burden states. Uninsured rates exceeded 12% vs. under 6%. Medicaid expansion was delayed. Since 2005, 193 rural hospitals have closed. Smoking rates were 21% vs. 10%; uncontrolled hypertension 30% vs. 18%.
Conclusions:
From 1999 to 2020, AAD mortality declined substantially but unevenly across sex, race, and geography. Disparities reflect access, coverage, and prevention gaps. Addressing these requires specialty expansion, rural hospital support, earlier Medicaid uptake, and community prevention.
Keywords: Aortic aneurysm; Aortic dissection; Mortality trends; Racial disparities; Geographic variation
More abstracts on this topic:
Adipocyte TRPM7 promotes aortic dissection by accelerating SMC phenotype switching
Wang Mi, Gao Min
A Machine Learning-Derived Socio-Environmental Risk Score More Accurately Predicts Cardiovascular Events and Better Addresses Health Inequities than Social Deprivation IndexChen Zhuo, Nasir Khurram, Al-kindi Sadeer, Rajagopalan Sanjay, Ponnana Sai Rahul, Dazard Jean-eudes, Zhang Tong, Dong Weichuan, Okyere Robert, Sirasapalli Santosh, Deo Salil, Khraishah Haitham