Final ID: MP890
Long-term outcomes of extensive aortic arch repair versus endovascular treatment in non-A non-B aortic dissection
Abstract Body (Do not enter title and authors here): Objective: This study presents a single-center retrospective analysis evaluating the long-term outcomes of patients with non-A non-B aortic dissection who underwent either total arch replacement with frozen elephant trunk (TAR with FET) or thoracic endovascular aortic repair (TEVAR).
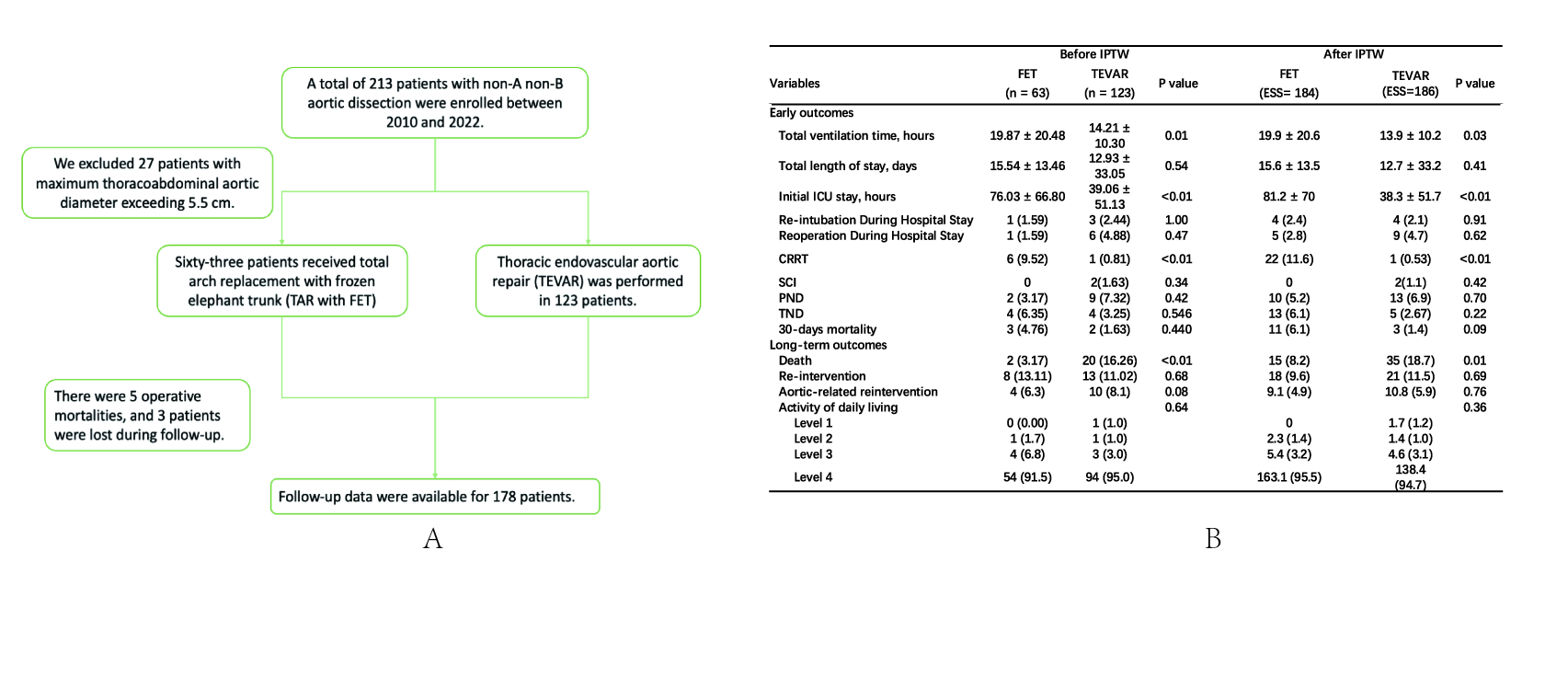
Methods: From 2010 to 2022, patients with non-A non-B aortic dissection who received TEVAR or TAR with FET were selected for clinical data collection and long-term follow-up. Baseline characteristics were balanced using inverse probability weighting.
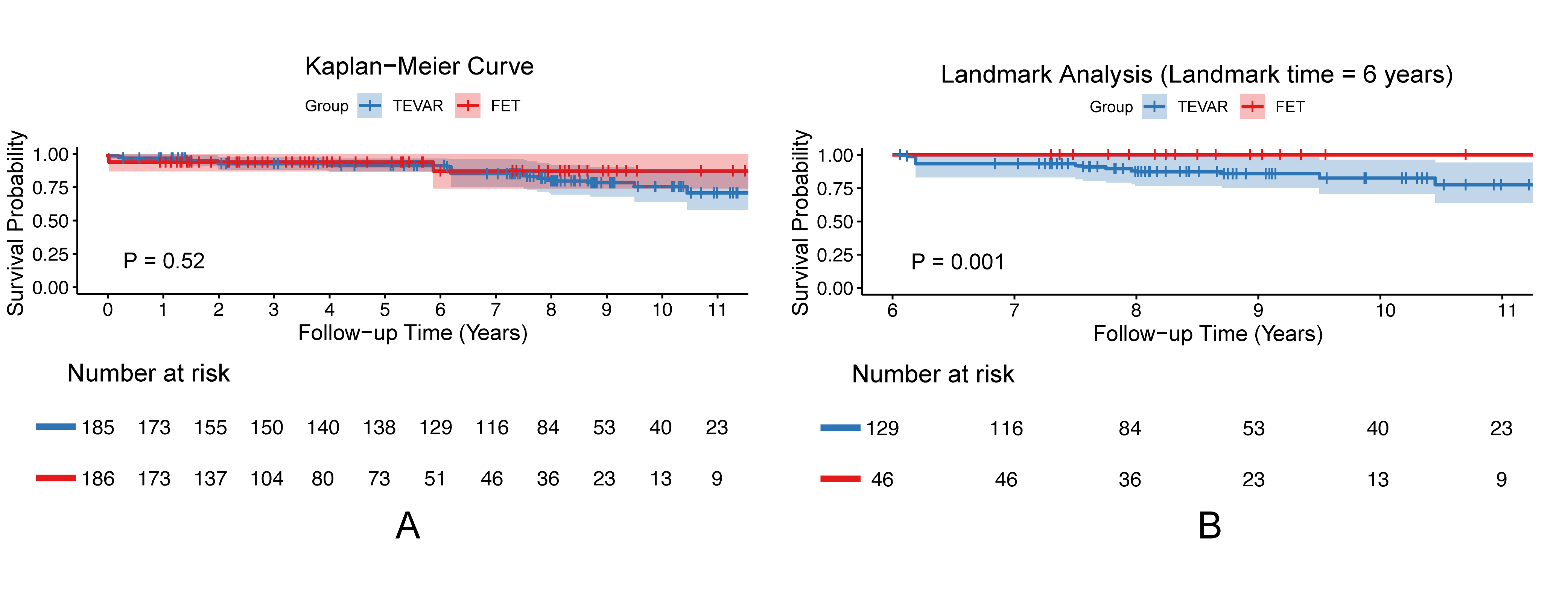
Result: A total of 186 patients were included, with 123 in the TEVAR group and 63 in the FET group. No significant difference in 30-day mortality was observed between the FET and TEVAR groups in both unadjusted and inverse probability weighting analyses (P > 0.05). The FET group, however, consistently showed higher rates of continuous renal replacement therapy (11.6% vs 0.53%, P<0.01) and prolonged intensive care unit stay (81.2 ± 70 h vs 38.3 ± 51.7 h, P<0.01). Kaplan-Meier curve analysis showed no significant difference in overall long-term survival (P > 0.05), but landmark analysis revealed that after 6 years post-operation, the FET group had significantly higher survival rates (P<0.01). Besides, there was no significant difference in aortic-related reintervention between groups (P > 0.05).
Conclusion: Regarding early prognosis, it is difficult to determine the superiority between these two approaches. However, from a long-term perspective, TAR with FET represents a more effective treatment strategy compared to TEVAR for patients with non-A non-B type aortic dissection.
Methods: From 2010 to 2022, patients with non-A non-B aortic dissection who received TEVAR or TAR with FET were selected for clinical data collection and long-term follow-up. Baseline characteristics were balanced using inverse probability weighting.
Result: A total of 186 patients were included, with 123 in the TEVAR group and 63 in the FET group. No significant difference in 30-day mortality was observed between the FET and TEVAR groups in both unadjusted and inverse probability weighting analyses (P > 0.05). The FET group, however, consistently showed higher rates of continuous renal replacement therapy (11.6% vs 0.53%, P<0.01) and prolonged intensive care unit stay (81.2 ± 70 h vs 38.3 ± 51.7 h, P<0.01). Kaplan-Meier curve analysis showed no significant difference in overall long-term survival (P > 0.05), but landmark analysis revealed that after 6 years post-operation, the FET group had significantly higher survival rates (P<0.01). Besides, there was no significant difference in aortic-related reintervention between groups (P > 0.05).
Conclusion: Regarding early prognosis, it is difficult to determine the superiority between these two approaches. However, from a long-term perspective, TAR with FET represents a more effective treatment strategy compared to TEVAR for patients with non-A non-B type aortic dissection.
More abstracts on this topic:
Impact of Surgical Selection on Stroke and Survival in Aortic Arch Aneurysm: A Risk-Adjusted Comparison Between Total Arch Replacement and Thoracic Endovascular Aortic Repair Using Najuta
Nishioka Naritomo, Kurimoto Yoshihiko, Ishige Hiroki, Yamamoto Mika, Masuda Takahiko, Maruyama Ryushi, Naraoka Shuichi
Changes in Management of Acute Aortic Syndrome with Vascular Medicine Involvement in a Multidisciplinary Aortic TeamPettinato Anthony, Milioglou Ioannis, Diggins Caroline, Krawisz Anna, Schmaier Alec, Secemsky Eric, Khabbaz Kamal, Schermerhorn Marc, Carroll Brett