Final ID: Su1144
Comparison of Short-Term Outcomes after Lower Extremity Bypass versus Peripheral Vascular Intervention in Patients with Chronic Limb-Threatening Ischemia and Diabetes Mellitus
Abstract Body (Do not enter title and authors here): Background: Comorbid diabetes mellitus (DM) is associated with worse outcomes in patients with chronic limb-threatening ischemia (CLTI). Both lower extremity bypass (LEB) and peripheral vascular interventions (PVI) have demonstrated improved outcomes in peripheral artery disease (PAD). However, comparative effectiveness data for LEB versus PVI in patients with CLTI and DM is limited.
Objective: This study aimed to evaluate and compare 30-day and 90-day (1) all-cause mortality, and (2) major amputation rates among patients with CLTI and comorbid DM undergoing LEB versus PVI.
Methods: Patients undergoing LEB and PVI were identified from the Vascular Quality Initiative registry, linked with Medicare claims outcomes data. Propensity scores were generated using 12 variables, and a 1:1 matching method was employed. The 30-day and 90-day mortality risks for LEB versus PVI were evaluated using Kaplan-Meier survival analysis and Cox proportional hazards models, incorporating interaction terms for DM. For amputation outcomes, cumulative incidence functions and Fine-Gray competing risks models were employed, with interaction terms for DM included.
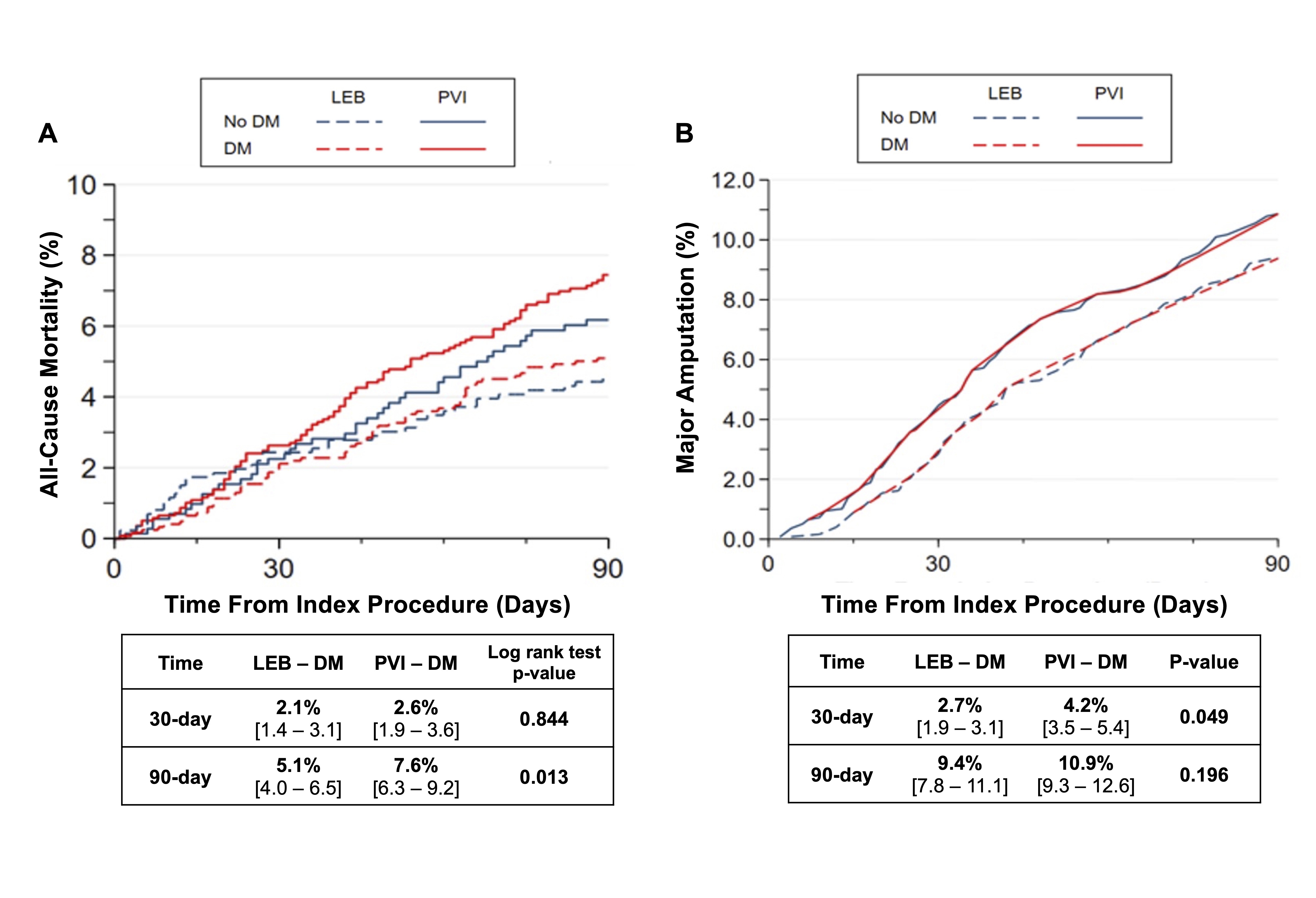
Results: Among 4,210 patients undergoing LEB or PVI (2,105 in each group), the mean age was 70.9 ± 10.9 years, with 69.3% being male and 76.4% white. DM was present in 62.3% (2,662 patients). In patients with DM, 30-day all-cause mortality rates were comparable between the LEB and PVI groups (2.1% vs. 2.6%; log-rank p-value=0.844). However, LEB was associated with significantly lower 90-day all-cause mortality rates compared to PVI (5.1% vs. 7.6%; log-rank p-value=0.013). Additionally, LEB was associated with a lower risk of 30-day major amputation rates compared to PVI (2.7% vs. 4.2%; p=0.049), though no significant difference was observed in 90-day major amputation rates (9.4% vs. 10.9%; p=0.196).
Conclusion: Among patients with CLTI and comorbid DM, LEB was associated with a lower risk of 30-day major amputation rates and 90-day all-cause mortality compared to PVI. These findings provide contemporary insights into the management of CLTI in diabetic patients, supporting informed shared decision-making for those often considered high-risk for surgical intervention.
Objective: This study aimed to evaluate and compare 30-day and 90-day (1) all-cause mortality, and (2) major amputation rates among patients with CLTI and comorbid DM undergoing LEB versus PVI.
Methods: Patients undergoing LEB and PVI were identified from the Vascular Quality Initiative registry, linked with Medicare claims outcomes data. Propensity scores were generated using 12 variables, and a 1:1 matching method was employed. The 30-day and 90-day mortality risks for LEB versus PVI were evaluated using Kaplan-Meier survival analysis and Cox proportional hazards models, incorporating interaction terms for DM. For amputation outcomes, cumulative incidence functions and Fine-Gray competing risks models were employed, with interaction terms for DM included.
Results: Among 4,210 patients undergoing LEB or PVI (2,105 in each group), the mean age was 70.9 ± 10.9 years, with 69.3% being male and 76.4% white. DM was present in 62.3% (2,662 patients). In patients with DM, 30-day all-cause mortality rates were comparable between the LEB and PVI groups (2.1% vs. 2.6%; log-rank p-value=0.844). However, LEB was associated with significantly lower 90-day all-cause mortality rates compared to PVI (5.1% vs. 7.6%; log-rank p-value=0.013). Additionally, LEB was associated with a lower risk of 30-day major amputation rates compared to PVI (2.7% vs. 4.2%; p=0.049), though no significant difference was observed in 90-day major amputation rates (9.4% vs. 10.9%; p=0.196).
Conclusion: Among patients with CLTI and comorbid DM, LEB was associated with a lower risk of 30-day major amputation rates and 90-day all-cause mortality compared to PVI. These findings provide contemporary insights into the management of CLTI in diabetic patients, supporting informed shared decision-making for those often considered high-risk for surgical intervention.
More abstracts on this topic:
Artificial Intelligence-Enabled Electrocardiography For The Prediction of Future Type 2 Diabetes Mellitus
Pastika Libor, Peters Nicholas, Kramer Daniel, Waks Jonathan, Sau Arunashis, Ng Fu Siong, Patlatzoglou Konstantinos, Sieliwonczyk Ewa, Barker Joseph, Zeidaabadi Boroumand, Mcgurk Kathryn, Khan Sadia, Mandic Danilo, Ware James
Changes in Management of Acute Aortic Syndrome with Vascular Medicine Involvement in a Multidisciplinary Aortic TeamPettinato Anthony, Milioglou Ioannis, Diggins Caroline, Krawisz Anna, Schmaier Alec, Secemsky Eric, Khabbaz Kamal, Schermerhorn Marc, Carroll Brett