Final ID: MP2311
Sleep Partially Mediates the Association Between Psychological and Cardiovascular Health Among Combat-exposed Service Members and Veterans
Abstract Body (Do not enter title and authors here): Background: Sleep disturbance is a common symptom of post-traumatic stress disorder (PTSD) and major depressive disorder (MDD) and is associated with poor cardiovascular health (CVH), especially in service members and veterans. Although sleep quality and obstructive sleep apnea are related, they represent distinct dimensions of sleep health. While sleep has been recognized as a component of CVH, the role of sleep quality and obstructive sleep apnea risk on the association between PTSD/MDD and CVH has received limited attention.
Research questions: Do sleep quality and risk for obstructive sleep apnea mediate the relationship between PTSD/MDD and CVH among the U.S. service members and veterans?
Methods: Cross-sectional analysis was conducted using the Long-Term Impact of Military-Relevant Brain Injury Consortium Chronic Effects of Neurotrauma Consortium (LIMBIC-CENC) study’s baseline data among combat-exposed members without a history of CVD. The PTSD/MDD group was identified if symptoms met the diagnostic criteria for either PTSD or MDD. Sleep quality was evaluated using the Pittsburgh Sleep Quality Index (scores 0-21), and high risk for obstructive sleep apnea was assessed using the STOP-Bang screening tool (yes vs. no). Blood pressure, glucose, lipids, body mass index, physical activity, and nicotine exposure were scored by Life’s Essential scoring metrics, with an unweighted average of the scores defined as CVH (ranging 0-100). Generalized linear regressions and mediation analysis with bootstrapping were used, adjusting for age, sex, race/ethnicity, and education.
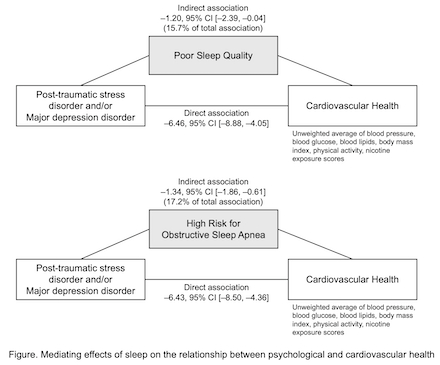
Results: Among 790 participants (mean age = 40 ± 9.4; 88% male; 54% non-Hispanic White), sleep quality significantly mediated the relationship between PTSD/MDD and CVH (indirect –1.20, 95% CI [–2.39, –0.04], direct –6.46, 95% CI [–8.88, –4.05]). High obstructive sleep apnea risk also showed a mediating effect on the relationship between PTSD/MDD and CVH (indirect –1.34, 95% CI [–1.86, –0.61], direct –6.43, 95% CI [–8.50, –4.36]). Sleep quality and obstructive sleep apnea risk accounted for approximately 15.7% and 17.2% of the total associations, respectively.
Conclusion: Poor sleep quality and high risk for obstructive sleep apnea partially mediate the relationship between PTSD/MDD and CVH, highlighting a meaningful pathway to intervene. Improving sleep among service members and veterans with PTSD or MDD may enhance CVH both directly and indirectly by reducing other cardiovascular risk factors.
Research questions: Do sleep quality and risk for obstructive sleep apnea mediate the relationship between PTSD/MDD and CVH among the U.S. service members and veterans?
Methods: Cross-sectional analysis was conducted using the Long-Term Impact of Military-Relevant Brain Injury Consortium Chronic Effects of Neurotrauma Consortium (LIMBIC-CENC) study’s baseline data among combat-exposed members without a history of CVD. The PTSD/MDD group was identified if symptoms met the diagnostic criteria for either PTSD or MDD. Sleep quality was evaluated using the Pittsburgh Sleep Quality Index (scores 0-21), and high risk for obstructive sleep apnea was assessed using the STOP-Bang screening tool (yes vs. no). Blood pressure, glucose, lipids, body mass index, physical activity, and nicotine exposure were scored by Life’s Essential scoring metrics, with an unweighted average of the scores defined as CVH (ranging 0-100). Generalized linear regressions and mediation analysis with bootstrapping were used, adjusting for age, sex, race/ethnicity, and education.
Results: Among 790 participants (mean age = 40 ± 9.4; 88% male; 54% non-Hispanic White), sleep quality significantly mediated the relationship between PTSD/MDD and CVH (indirect –1.20, 95% CI [–2.39, –0.04], direct –6.46, 95% CI [–8.88, –4.05]). High obstructive sleep apnea risk also showed a mediating effect on the relationship between PTSD/MDD and CVH (indirect –1.34, 95% CI [–1.86, –0.61], direct –6.43, 95% CI [–8.50, –4.36]). Sleep quality and obstructive sleep apnea risk accounted for approximately 15.7% and 17.2% of the total associations, respectively.
Conclusion: Poor sleep quality and high risk for obstructive sleep apnea partially mediate the relationship between PTSD/MDD and CVH, highlighting a meaningful pathway to intervene. Improving sleep among service members and veterans with PTSD or MDD may enhance CVH both directly and indirectly by reducing other cardiovascular risk factors.
More abstracts on this topic:
AHA Life's essential 8 and ideal cardiovascular health among adult swimmers
Tiozzo Eduard, Henley Cynthia, Jones Caroline, Perry Fredrick, Viscovich Isabella, Johnson Giana, Gardener Hannah, Yu Kerstin
Association of Atrial Fibrillation with Lamotrigine in Bipolar I Disorder: An Observational Cohort StudyKim Sodam, Welch Landon, De Los Santos Bertha, Radwanski Przemyslaw, Kim Kibum, Munger Mark