Final ID: Su1132
Association of depression symptoms with cardiovascular health stratified by military status: Insights from 2013-2020 National Health and Nutrition Examination Survey
Abstract Body (Do not enter title and authors here): Introduction: Emerging evidence supports the mind-heart-body connection, yet less attention has been given to examining the relationship in specific populations. Veterans have a higher risk for mental and cardiovascular problems and have unique social determinants of health (SDoH), such as healthcare access, than civilians. This study aims to examine how depression and SDoH are associated with cardiovascular health (CVH) and if associations differ by military status.
Hypotheses: 1) Depression symptoms and SDoH will be associated with CVH. 2) The associations will differ between people who served in the US military and those who did not.
Methods: A cross-sectional analysis was conducted using data from the 2013 to 2020 National Health and Nutrition Examination Survey. Individuals were aged ≥ 20 years without cardiovascular disease and current pregnancy. Patient Health Questionnaire-9 was used to assess depression symptoms and dichotomized into no symptoms (<5) and mild-to-severe symptoms (≥5). The Life's Essential 8 quantified CVH, with scores from 0-100. SDoH included age, gender, race/ethnicity, marital status, education, employment, financial status, health insurance, and healthcare access. Sample weights were applied in multiple linear regression analyses.
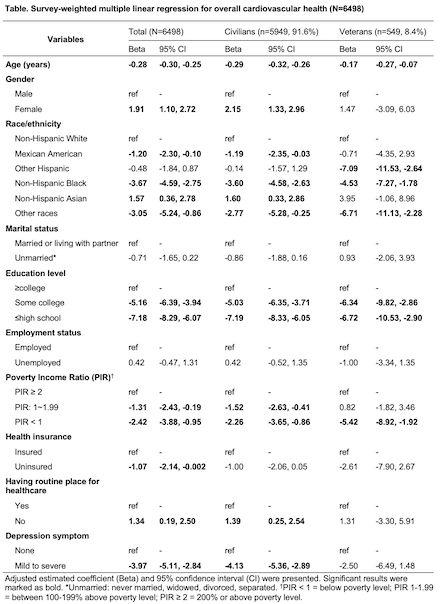
Results: Among 6498 participants, 92% were civilians (mean age: 45 years; 51% female), and 8% were veterans (mean age: 56 years; 10% female). In both groups, 23% had depression symptoms. The mean CVH was 72 in civilians and 69 in veterans. In adjusted models, individuals with depression symptoms had 4 points lower CVH scores than those without (95% CI: -5.11, -2.84). This trend was similar in civilians but insignificant in veterans. Lower CVH was significantly associated with age, being non-Hispanic Black and other races people, lower education, and lower financial status. The associations were preserved after being stratified by military status.
Conclusions: Depression symptoms and SDoH were associated with lower CVH. However, there was no significant evidence that military status moderated the associations of depression and SDoH with CVH. Examining the intersection between depressive symptoms and SDoH may be useful when assessing CVH.
Hypotheses: 1) Depression symptoms and SDoH will be associated with CVH. 2) The associations will differ between people who served in the US military and those who did not.
Methods: A cross-sectional analysis was conducted using data from the 2013 to 2020 National Health and Nutrition Examination Survey. Individuals were aged ≥ 20 years without cardiovascular disease and current pregnancy. Patient Health Questionnaire-9 was used to assess depression symptoms and dichotomized into no symptoms (<5) and mild-to-severe symptoms (≥5). The Life's Essential 8 quantified CVH, with scores from 0-100. SDoH included age, gender, race/ethnicity, marital status, education, employment, financial status, health insurance, and healthcare access. Sample weights were applied in multiple linear regression analyses.
Results: Among 6498 participants, 92% were civilians (mean age: 45 years; 51% female), and 8% were veterans (mean age: 56 years; 10% female). In both groups, 23% had depression symptoms. The mean CVH was 72 in civilians and 69 in veterans. In adjusted models, individuals with depression symptoms had 4 points lower CVH scores than those without (95% CI: -5.11, -2.84). This trend was similar in civilians but insignificant in veterans. Lower CVH was significantly associated with age, being non-Hispanic Black and other races people, lower education, and lower financial status. The associations were preserved after being stratified by military status.
Conclusions: Depression symptoms and SDoH were associated with lower CVH. However, there was no significant evidence that military status moderated the associations of depression and SDoH with CVH. Examining the intersection between depressive symptoms and SDoH may be useful when assessing CVH.
More abstracts on this topic:
A Finding of Unique Peak Exercise Level in Respiratory Exchange Ratio during Bicycle Ergometric Cardiopulmonary Exercise Testing in Healthy Subjects
Nakayama Atsuko, Sakuma Hiroki, Iwata Tomoharu, Kashino Kunio, Isobe Mitsuaki, Tomoike Hitonobu
Bleeding Risks for Acute Ischemic Stroke Patients on Serotonergic Antidepressants and Anticoagulation/Dual Anti-Platelet TherapySimmonds Kent, Chavez Audrie, Ifejika Nneka