Final ID: MP2524
Systemwide Implementation of Bridge Clinics Reduces Readmissions and Hospital Utilization in Urban and Rural Heart Failure Populations
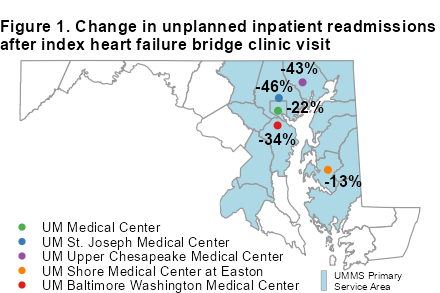
Abstract Body (Do not enter title and authors here): Background: Heart Failure (HF) is a leading cause of 30-day readmissions (20-25% nationally). Interdisciplinary Bridge Clinics (BCs) improve continuity of care, reduce readmissions, and shift care from high-cost inpatient settings to more sustainable outpatient management. The University of Maryland Medical System (UMMS) launched its first BC in 2015 at its quaternary care academic hospital in Baltimore. Since then, four additional clinics have been established across UMMS, most recently in 2024, expanding HF care access in urban and rural areas (Figure 1). This study evaluates whether similar benefits seen at the original site—reduced readmissions and utilization—are observed at new clinics across the health system.
Methods: In this retrospective observational cohort study, we analyzed patients from five UMMS hospitals who attended a BC between January and November 2024. The index event was the first BC visit. Healthcare utilization was assessed using the Chesapeake Regional Information System for our Patients (CRISP) Visit Level Pre/Post Analysis tool, examining up to 12 months before and after the index visit. We analyzed inpatient, observation, emergency department (ED), and outpatient visits, and 30-day readmissions, using CMS criteria to exclude planned hospitalizations.
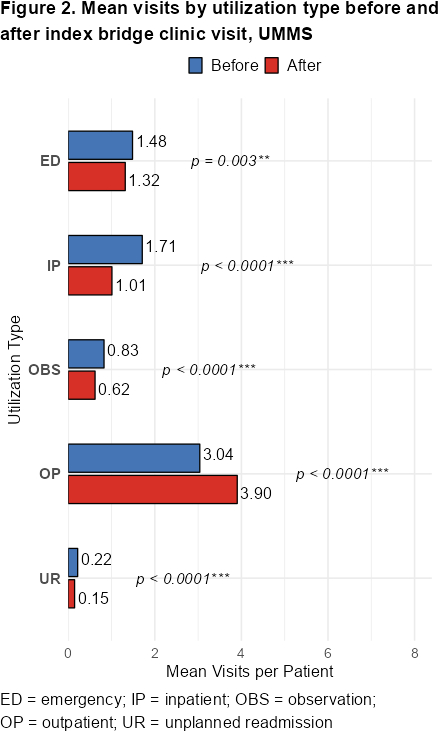
HF subtype was categorized using ICD-10 codes. Utilization changes were analyzed with the Wilcoxon signed-rank test; results by HF subtype and site are presented descriptively (Figure 2).
Results: Each site showed a reduction in inpatient readmissions after BC (Figure 1). Pooled data across all 5 system sites showed statistically that inpatient utilization decreased by 41% (p<0.001), outpatient utilization increased by 28.5% (p<0.001) and readmissions decreased by 32.7% (p<0.001) (Figure 2).
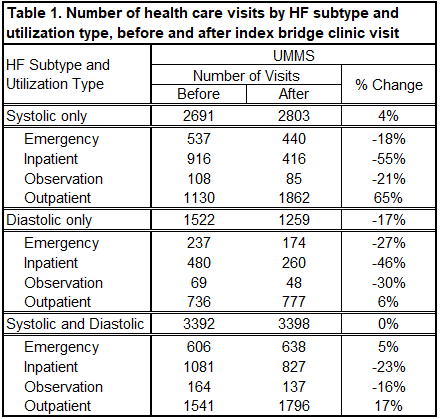
Improved outcomes were evident across the HF spectrum (Table 1). Patients with all HF types had fewer admissions and ED visits following BC visit. This trend was seen across all 5 sites.
Conclusion: Implementation of transitional BCs across a diverse urban and rural hospital system was associated with reductions in utilization and readmissions, with increased outpatient engagement. These improvements were consistent across all HF subtypes. System-wide adoption of post-discharge interdisciplinary follow-up via BCs can improve care transitions and reduce care utilization in HF populations, regardless of setting. Future studies should assess long-term outcomes, cost-effectiveness, and equitable access.
Methods: In this retrospective observational cohort study, we analyzed patients from five UMMS hospitals who attended a BC between January and November 2024. The index event was the first BC visit. Healthcare utilization was assessed using the Chesapeake Regional Information System for our Patients (CRISP) Visit Level Pre/Post Analysis tool, examining up to 12 months before and after the index visit. We analyzed inpatient, observation, emergency department (ED), and outpatient visits, and 30-day readmissions, using CMS criteria to exclude planned hospitalizations.
HF subtype was categorized using ICD-10 codes. Utilization changes were analyzed with the Wilcoxon signed-rank test; results by HF subtype and site are presented descriptively (Figure 2).
Results: Each site showed a reduction in inpatient readmissions after BC (Figure 1). Pooled data across all 5 system sites showed statistically that inpatient utilization decreased by 41% (p<0.001), outpatient utilization increased by 28.5% (p<0.001) and readmissions decreased by 32.7% (p<0.001) (Figure 2).
Improved outcomes were evident across the HF spectrum (Table 1). Patients with all HF types had fewer admissions and ED visits following BC visit. This trend was seen across all 5 sites.
Conclusion: Implementation of transitional BCs across a diverse urban and rural hospital system was associated with reductions in utilization and readmissions, with increased outpatient engagement. These improvements were consistent across all HF subtypes. System-wide adoption of post-discharge interdisciplinary follow-up via BCs can improve care transitions and reduce care utilization in HF populations, regardless of setting. Future studies should assess long-term outcomes, cost-effectiveness, and equitable access.
More abstracts on this topic:
Early Post Acute Care Pathways are Predictive of 1-Year Home Time among Patients with Acute Ischemic Stroke: Analysis of Clinical and Claims Linked Data
Pan Alan, Kim Yejin, Jiang Xiaoqian, Vahidy Farhaan, Wozny Joseph, Schaefer Caroline, Bako Abdulaziz, Nicolas Charlie, Potter Thomas, Caballero Elizabeth, Nair Rejani, Ganduglia-cazaban Cecilia
Educational support in the transitional care: a qualitative meta-synthesis of the experiences of caregiver-stroke survivor dyadsPetrosino Francesco, Bartoli Davide, Trotta Francesca, Vellone Ercole, Alvaro Rosaria, Pucciarelli Gianluca