Final ID: MP460
Temporal Trends in Major Adverse Cardiovascular Events Following Hospitalization for Myocardial Infarction Between 2008-2022: Insights from the Veterans Affairs Healthcare System
Abstract Body (Do not enter title and authors here): Background:
Over 800,000 individuals are hospitalized for a myocardial infarction (MI) annually in the United States. Temporal trends in post-discharge outcomes are uncertain.
Question:
Among Veterans who survive an MI hospitalization, how have post-discharge outcomes changed?
Methods:
Veterans who survived an MI hospitalization within or outside the VHA between 2008-2022 were identified based on a principal diagnosis of MI from an acute care hospitalization. We identified comorbidities, vital signs, and laboratory values pre-hospitalization.
The primary outcome was a 4-point composite MACE (death, MI, ischemic stroke, and heart failure (HF) hospitalization) over 1 year post-discharge. Temporal trends were analyzed by comparing outcomes across 3 time periods (2008-2012, 2013-2017, and 2018-2022) with the Cuzick rank test. We also evaluated 1-year death alone and performed a landmark analysis evaluating 1-year death following HF hospitalization within the first 12 months post-MI. The annual change in outcomes was examined while adjusting for demographics, comorbidities, pre-admission vital signs and laboratory values, and STEMI vs. NSTEMI classification.
Results:
There were 444,659 Veterans with a non-fatal MI hospitalization between 2008 and 2022. The median age was 73 (interquartile range: 66-80) and 1.8% were women. Over time, the proportion with STEMI decreased (2008-2012: 26.1%, 2013-2017: 23.1%, and 2018-2022: 23.1%; p<0.01). The proportion with inpatient revascularization decreased from 49.6% to 48.1% to 36.9% (p<0.01).
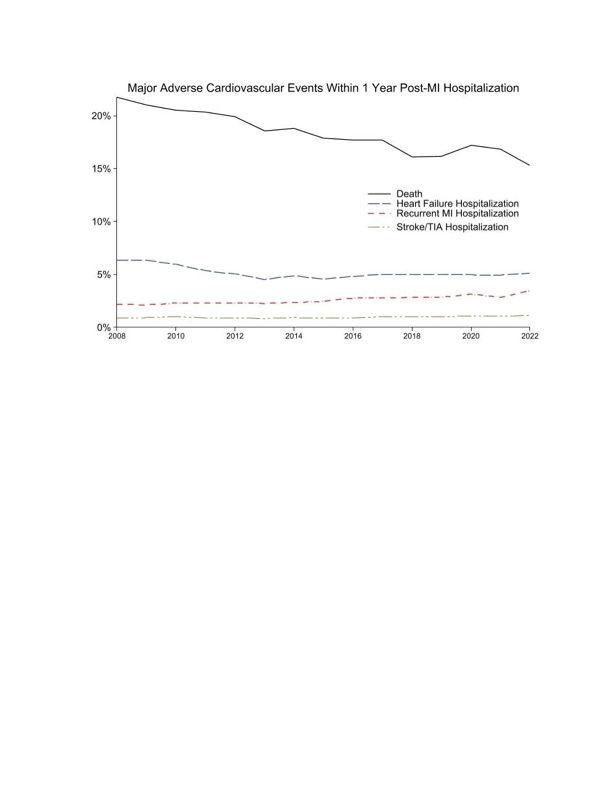
The 1-year risk of the composite MACE outcome decreased from 26.1% to 23.2% to 22.2% (p<0.01) across time periods. After adjustment, there was a 3.9% annual relative decrease in the odds of 1-year MACE (OR: 0.965; 95% CI: 0.963-0.967). The risk of 1-year death post-MI hospitalization decreased from 20.7% to 18.1% to 16.3% (p<0.01) (Figure). After adjustment, there was a 4.2% annual relative decrease in the odds of 1-year mortality (OR 0.958 per year; 95% CI: 0.956-0.960).
There were 23,048 (5.2%) Veterans with HF hospitalization within 12 months of MI discharge. Among this cohort, 44.9% died within 1-year post-HF hospitalization.
Conclusion:
Among Veterans, the risk of death post-MI hospitalization has improved over time. However, over 1 in 5 Veterans post-MI continue to have major adverse cardiovascular outcomes within 1 year. Veterans with a HF hospitalization post-MI are at substantially elevated risk of death.
Over 800,000 individuals are hospitalized for a myocardial infarction (MI) annually in the United States. Temporal trends in post-discharge outcomes are uncertain.
Question:
Among Veterans who survive an MI hospitalization, how have post-discharge outcomes changed?
Methods:
Veterans who survived an MI hospitalization within or outside the VHA between 2008-2022 were identified based on a principal diagnosis of MI from an acute care hospitalization. We identified comorbidities, vital signs, and laboratory values pre-hospitalization.
The primary outcome was a 4-point composite MACE (death, MI, ischemic stroke, and heart failure (HF) hospitalization) over 1 year post-discharge. Temporal trends were analyzed by comparing outcomes across 3 time periods (2008-2012, 2013-2017, and 2018-2022) with the Cuzick rank test. We also evaluated 1-year death alone and performed a landmark analysis evaluating 1-year death following HF hospitalization within the first 12 months post-MI. The annual change in outcomes was examined while adjusting for demographics, comorbidities, pre-admission vital signs and laboratory values, and STEMI vs. NSTEMI classification.
Results:
There were 444,659 Veterans with a non-fatal MI hospitalization between 2008 and 2022. The median age was 73 (interquartile range: 66-80) and 1.8% were women. Over time, the proportion with STEMI decreased (2008-2012: 26.1%, 2013-2017: 23.1%, and 2018-2022: 23.1%; p<0.01). The proportion with inpatient revascularization decreased from 49.6% to 48.1% to 36.9% (p<0.01).
The 1-year risk of the composite MACE outcome decreased from 26.1% to 23.2% to 22.2% (p<0.01) across time periods. After adjustment, there was a 3.9% annual relative decrease in the odds of 1-year MACE (OR: 0.965; 95% CI: 0.963-0.967). The risk of 1-year death post-MI hospitalization decreased from 20.7% to 18.1% to 16.3% (p<0.01) (Figure). After adjustment, there was a 4.2% annual relative decrease in the odds of 1-year mortality (OR 0.958 per year; 95% CI: 0.956-0.960).
There were 23,048 (5.2%) Veterans with HF hospitalization within 12 months of MI discharge. Among this cohort, 44.9% died within 1-year post-HF hospitalization.
Conclusion:
Among Veterans, the risk of death post-MI hospitalization has improved over time. However, over 1 in 5 Veterans post-MI continue to have major adverse cardiovascular outcomes within 1 year. Veterans with a HF hospitalization post-MI are at substantially elevated risk of death.
More abstracts on this topic:
A New Analytical Approach for Noninvasive Reconstruction of the Entire Left Ventricular Pressure Waveform in Myocardial Ischemia and Infarction
Bilgi Coskun, Li Jiajun, Alavi Rashid, Dai Wangde, Matthews Ray, Kloner Robert, Pahlevan Niema
A 50% or Greater Reduction in LDL-Cholesterol Is Associated with Improved Long-Term Outcomes and Lower Health Care Utilization After Myocardial Infarction - a SWEDEHEART studyReitan Christian, Watanabe Alexandre, Bash Lori, Galvain Thibaut, Arnet Urs, Jernberg Tomas