Final ID: MP458
Clinical Outcomes Among Individuals with Persistent Systemic Inflammation Following Myocardial Infarction: Insights from the Veterans Affairs Healthcare System
Abstract Body (Do not enter title and authors here):
Introduction
Acute myocardial infarction (MI) triggers acute inflammation. A subset of patients experience subsequent chronic systemic inflammation (SI) post-MI.
Question
Among patients with a prior MI, is SI associated with a higher risk of major adverse cardiovascular (CV) events?
Methods
We identified Veterans with a nonfatal MI from 2008-2022 and a subsequent outpatient high-sensitivity C-reactive protein (hsCRP) measurement 60-730 days post-MI. Veterans with select comorbidities known to increase SI and mortality (e.g., active cancer or end-stage renal or severe hepatic diseases) were excluded.
The primary outcome was a composite of death, MI, and ischemic stroke post-hsCRP measurement. Secondary outcomes included components of the primary outcome, CV death, and heart failure (HF) hospitalization. Cox regression was used to compare outcomes between patients with SI (hsCRP >2 mg/L and <10 mg/L) vs. without SI (hsCRP <2 mg/L), adjusting for demographics, comorbidities, CV treatment (statins, antiplatelets, GLP1RA, and SGLT2i), and the duration between MI and hsCRP.
Results
We identified 11,230 Veterans with a nonfatal MI with a subsequent hsCRP: 3,362 had hsCRP <2 mg/L, 4,594 had hsCRP >2 mg/L and <10 mg/L, and 3,274 had hsCRP >10 mg/L. Among Veterans with hsCRP <10 mg/L, the mean age was 68 years (SD: 9.7), 96.8% were men, 73.2% had NSTEMI, and 55.6% underwent coronary revascularization. Veterans with SI were more likely to have diabetes (41.1% vs. 33.0%, p<0.001) compared to those without SI.
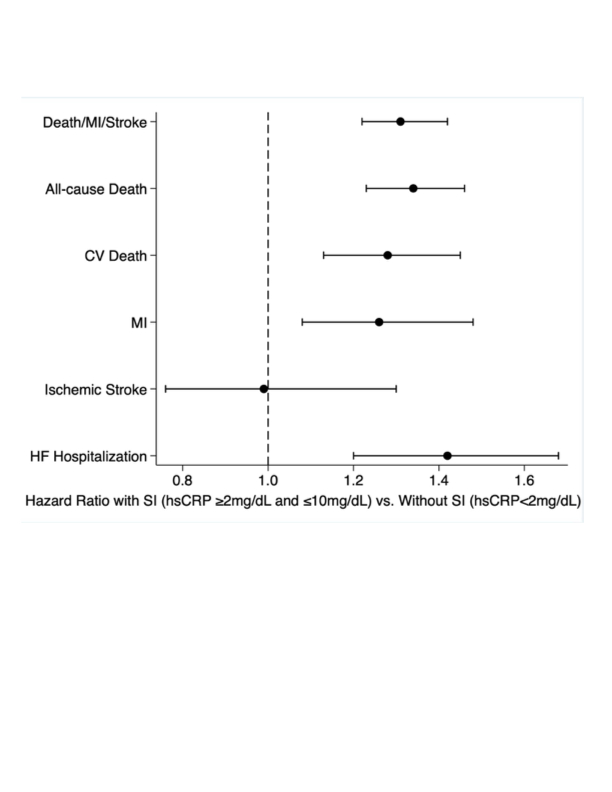
The composite outcome incidence was 7.2 events/100 patient-years in those with SI vs. 5.0/100 patient-years in those without SI (p<0.001). After adjustment, SI was associated with a higher risk of the primary outcome (HR: 1.31; 95% CI: 1.22–1.42). SI was also associated with an increased risk of each of the following: all-cause death, CV death, recurrent MI, and HF hospitalization (Figure 1). The results were similar after excluding patients with autoimmune disease and across subgroups by age, diabetes, heart failure, and NSTEMI vs. STEMI.
Conclusion
SI following a nonfatal MI is a marker of increased risk of death, recurrent MI, and HF hospitalizations after adjustment for patient demographics, comorbidities, and CV treatment.
Introduction
Acute myocardial infarction (MI) triggers acute inflammation. A subset of patients experience subsequent chronic systemic inflammation (SI) post-MI.
Question
Among patients with a prior MI, is SI associated with a higher risk of major adverse cardiovascular (CV) events?
Methods
We identified Veterans with a nonfatal MI from 2008-2022 and a subsequent outpatient high-sensitivity C-reactive protein (hsCRP) measurement 60-730 days post-MI. Veterans with select comorbidities known to increase SI and mortality (e.g., active cancer or end-stage renal or severe hepatic diseases) were excluded.
The primary outcome was a composite of death, MI, and ischemic stroke post-hsCRP measurement. Secondary outcomes included components of the primary outcome, CV death, and heart failure (HF) hospitalization. Cox regression was used to compare outcomes between patients with SI (hsCRP >2 mg/L and <10 mg/L) vs. without SI (hsCRP <2 mg/L), adjusting for demographics, comorbidities, CV treatment (statins, antiplatelets, GLP1RA, and SGLT2i), and the duration between MI and hsCRP.
Results
We identified 11,230 Veterans with a nonfatal MI with a subsequent hsCRP: 3,362 had hsCRP <2 mg/L, 4,594 had hsCRP >2 mg/L and <10 mg/L, and 3,274 had hsCRP >10 mg/L. Among Veterans with hsCRP <10 mg/L, the mean age was 68 years (SD: 9.7), 96.8% were men, 73.2% had NSTEMI, and 55.6% underwent coronary revascularization. Veterans with SI were more likely to have diabetes (41.1% vs. 33.0%, p<0.001) compared to those without SI.
The composite outcome incidence was 7.2 events/100 patient-years in those with SI vs. 5.0/100 patient-years in those without SI (p<0.001). After adjustment, SI was associated with a higher risk of the primary outcome (HR: 1.31; 95% CI: 1.22–1.42). SI was also associated with an increased risk of each of the following: all-cause death, CV death, recurrent MI, and HF hospitalization (Figure 1). The results were similar after excluding patients with autoimmune disease and across subgroups by age, diabetes, heart failure, and NSTEMI vs. STEMI.
Conclusion
SI following a nonfatal MI is a marker of increased risk of death, recurrent MI, and HF hospitalizations after adjustment for patient demographics, comorbidities, and CV treatment.
More abstracts on this topic:
A Machine Learning Readmission Risk Prediction Model for Cardiac Disease
Bailey Angela, Wang Wei, Shannon Clarence, Huling Jared, Tignanelli Christopher
A 50% or Greater Reduction in LDL-Cholesterol Is Associated with Improved Long-Term Outcomes and Lower Health Care Utilization After Myocardial Infarction - a SWEDEHEART studyReitan Christian, Watanabe Alexandre, Bash Lori, Galvain Thibaut, Arnet Urs, Jernberg Tomas