Final ID: MP758
Time-Dependent Impact of the 2018 UNOS Heart Allocation Policy Revision on Transplantation and Waitlist Outcomes: A Landmark Competing Risks Analysis
Abstract Body (Do not enter title and authors here):
Background:
While early data following the 2018 United Network for Organ Sharing (UNOS) heart allocation policy revision showed improved transplantation rates and reduced waitlist mortality, it is unclear how these effects may affect a population through time of interaction with the policy.
Research Question:
To evaluate the impact of the 2018 UNOS allocation policy change on heart transplant candidate outcomes at predefined landmark times.
Methods:
This was a retrospective competing risks analysis of pre- and post-policy patients at 0, 2, 4, 8, 16, and 24 weeks post-listing using UNOS registry data. We included adults listed for heart-only, heart-kidney, or heart-liver transplantation between 10/18/2018 and 08/30/2023, separated into high- or low-acuity based on waitlist status. Time-varying subdistribution (sdHR) and cause-specific hazard ratios (csHR) for heart transplantation, death or clinical deterioration, and myocardial recovery were calculated.
Results:
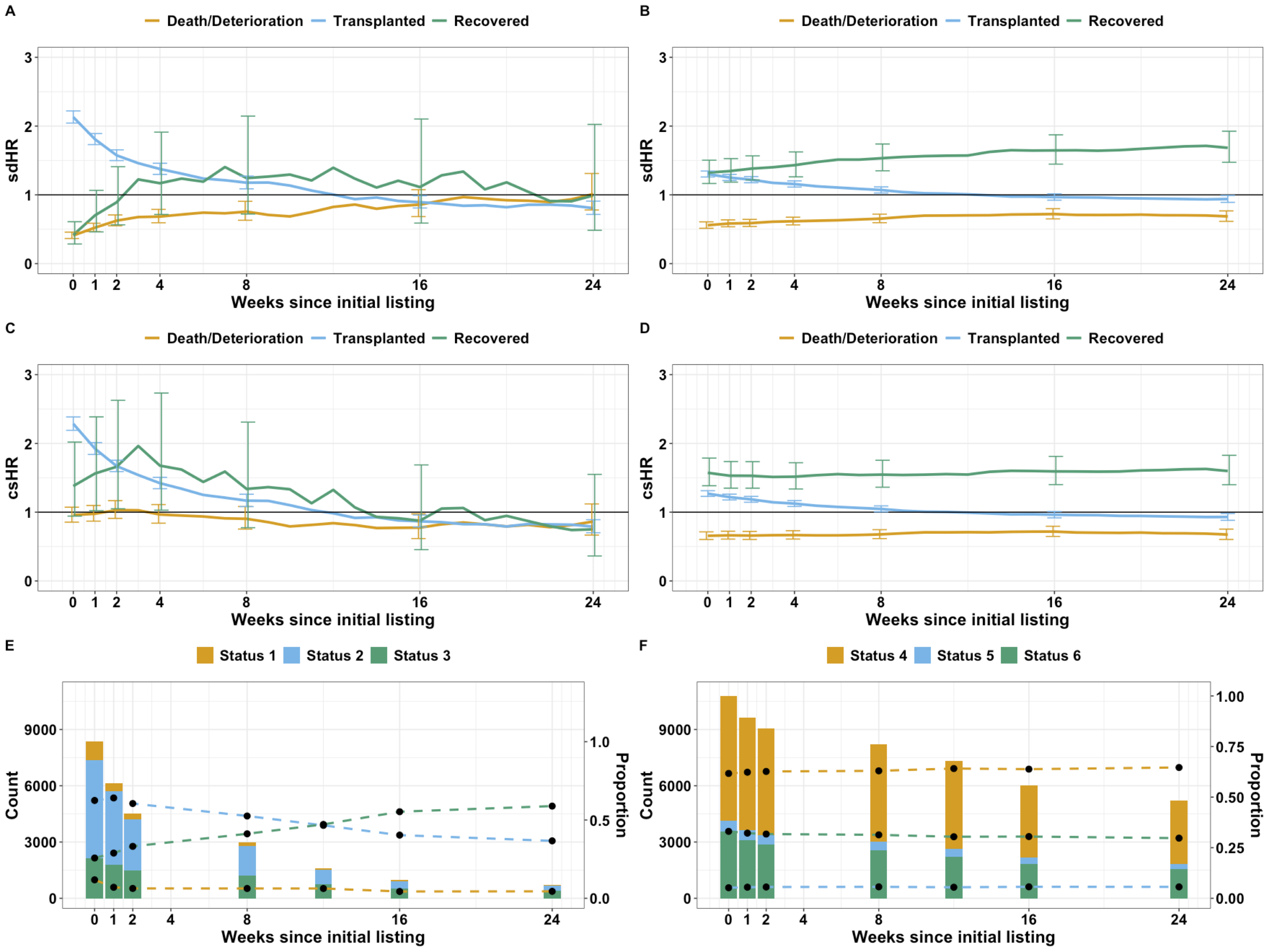
We included 35,520 patients, with 16,357 pre-policy (high-acuity: 4,121, low-acuity: 12,236) and 19,163 post-policy (high-acuity: 8,199, low-acuity: 10,964). Among high-acuity patients, heart transplantation rates were significantly higher post-policy early on (week 0 sdHR: 2.13; 95% CI: 2.04, 2.22; p<0.001) but decreased over time (week 16 sdHR: 0.89; 95% CI: 0.81, 0.99; p=0.027). Protection from death/deterioration post-policy (week 0 sdHR: 0.41; 95% CI: 0.37, 0.46; p<0.001) also diminished over time (week 24 sdHR: 1.01 (95% CI: 0.78, 1.31; p=0.93) (Figure 1).
Among low-acuity patients, initial elevated heart transplantation rates (week 0 sdHR 1.30, 95% CI: 1.26, 1.35; p<0.001) declined over time (week 24 sdHR: 0.94; 95% CI: 0.89, 0.99; p=0.022). However, there was a sustained reduction in death/deterioration risk (week 0 sdHR 0.56; 95% CI: 0.51, 0.61; p<0.001 vs. week 24 sdHR 0.69; 95% CI: 0.62, 0.77; p<0.001) and increased likelihood of myocardial recovery (week 0 sdHR 1.32; 95% CI: 1.17, 1.50; p<0.001 vs. week 24 sdHR 1.68; 95% CI: 1.47, 1.93; p<0.001) (Figure 2).
Conclusion:
After a period between 12-16 weeks, transplant likelihood in both groups fell below that of the prior policy, as did the chance of recovery in high-acuity patients. While higher acuity transplantation rates can be explained by Status 1 patients being transplanted sooner, the same cannot be said for the low-acuity patients. Our findings suggest that the benefits of the new policy are not universal nor static across waitlist time.
Background:
While early data following the 2018 United Network for Organ Sharing (UNOS) heart allocation policy revision showed improved transplantation rates and reduced waitlist mortality, it is unclear how these effects may affect a population through time of interaction with the policy.
Research Question:
To evaluate the impact of the 2018 UNOS allocation policy change on heart transplant candidate outcomes at predefined landmark times.
Methods:
This was a retrospective competing risks analysis of pre- and post-policy patients at 0, 2, 4, 8, 16, and 24 weeks post-listing using UNOS registry data. We included adults listed for heart-only, heart-kidney, or heart-liver transplantation between 10/18/2018 and 08/30/2023, separated into high- or low-acuity based on waitlist status. Time-varying subdistribution (sdHR) and cause-specific hazard ratios (csHR) for heart transplantation, death or clinical deterioration, and myocardial recovery were calculated.
Results:
We included 35,520 patients, with 16,357 pre-policy (high-acuity: 4,121, low-acuity: 12,236) and 19,163 post-policy (high-acuity: 8,199, low-acuity: 10,964). Among high-acuity patients, heart transplantation rates were significantly higher post-policy early on (week 0 sdHR: 2.13; 95% CI: 2.04, 2.22; p<0.001) but decreased over time (week 16 sdHR: 0.89; 95% CI: 0.81, 0.99; p=0.027). Protection from death/deterioration post-policy (week 0 sdHR: 0.41; 95% CI: 0.37, 0.46; p<0.001) also diminished over time (week 24 sdHR: 1.01 (95% CI: 0.78, 1.31; p=0.93) (Figure 1).
Among low-acuity patients, initial elevated heart transplantation rates (week 0 sdHR 1.30, 95% CI: 1.26, 1.35; p<0.001) declined over time (week 24 sdHR: 0.94; 95% CI: 0.89, 0.99; p=0.022). However, there was a sustained reduction in death/deterioration risk (week 0 sdHR 0.56; 95% CI: 0.51, 0.61; p<0.001 vs. week 24 sdHR 0.69; 95% CI: 0.62, 0.77; p<0.001) and increased likelihood of myocardial recovery (week 0 sdHR 1.32; 95% CI: 1.17, 1.50; p<0.001 vs. week 24 sdHR 1.68; 95% CI: 1.47, 1.93; p<0.001) (Figure 2).
Conclusion:
After a period between 12-16 weeks, transplant likelihood in both groups fell below that of the prior policy, as did the chance of recovery in high-acuity patients. While higher acuity transplantation rates can be explained by Status 1 patients being transplanted sooner, the same cannot be said for the low-acuity patients. Our findings suggest that the benefits of the new policy are not universal nor static across waitlist time.
More abstracts on this topic:
Analysis of 30-Day Readmission Rates and Costs Post-Heart Transplant: A 12-Year Retrospective Study Using Nationwide Readmission Database(NRD) : 2010-2021
Pinninty Dheeraj, Mogga Phanidhar, Raol Karanrajsinh, Pillai Ashwin, Mudduluru Prathyusha, Singh Kerry, Jedeon Zeina, Jaiswal Abhishek
Application of Artificial Intelligence (AI) for Predictive Modelling and Imaging in Cardiac Transplantation - A Systematic Review and Meta-AnalysisIyer Vardhini Ganesh, Chandra Mohan Trisha, Gupta Aryan, Gupta Era, Prasad Kushal, Kalra Shekhar, Chandramouli Bellur Vinay, Prasad Ananya, Oudit Omar, Magaji Rishikesh R