Final ID: MP1956
A RARE CARDIAC COMPLICATION OF LEGIONNAIRES' DISEASE: LEFT VENTRICULAR APICAL THROMBUS WITH SEVERE CARDIOMYOPATHY
Abstract Body (Do not enter title and authors here): Introduction: Legionnaires’ disease, caused by Legionella pneumophila, primarily manifests as severe pneumonia but can lead to rare cardiac complications. Left ventricular (LV) thrombus formation is uncommon and typically occurs in the presence of severe LV dysfunction, systemic inflammation, and hypercoagulability. We present a case of LV mural thrombus in a 62 year old patient with Legionnaires’ disease, emphasizing the importance of recognizing cardiovascular involvement in severe infections.
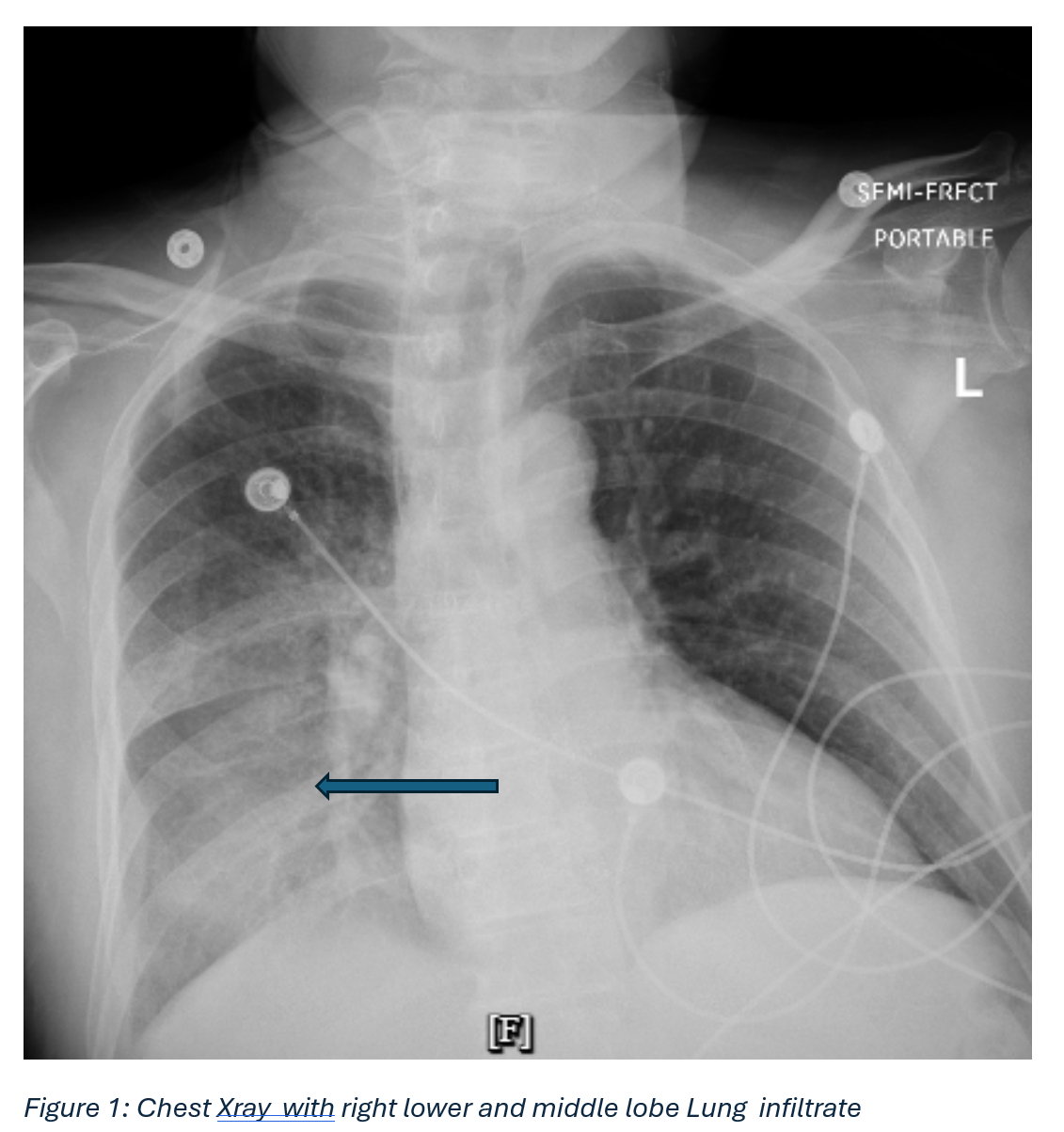
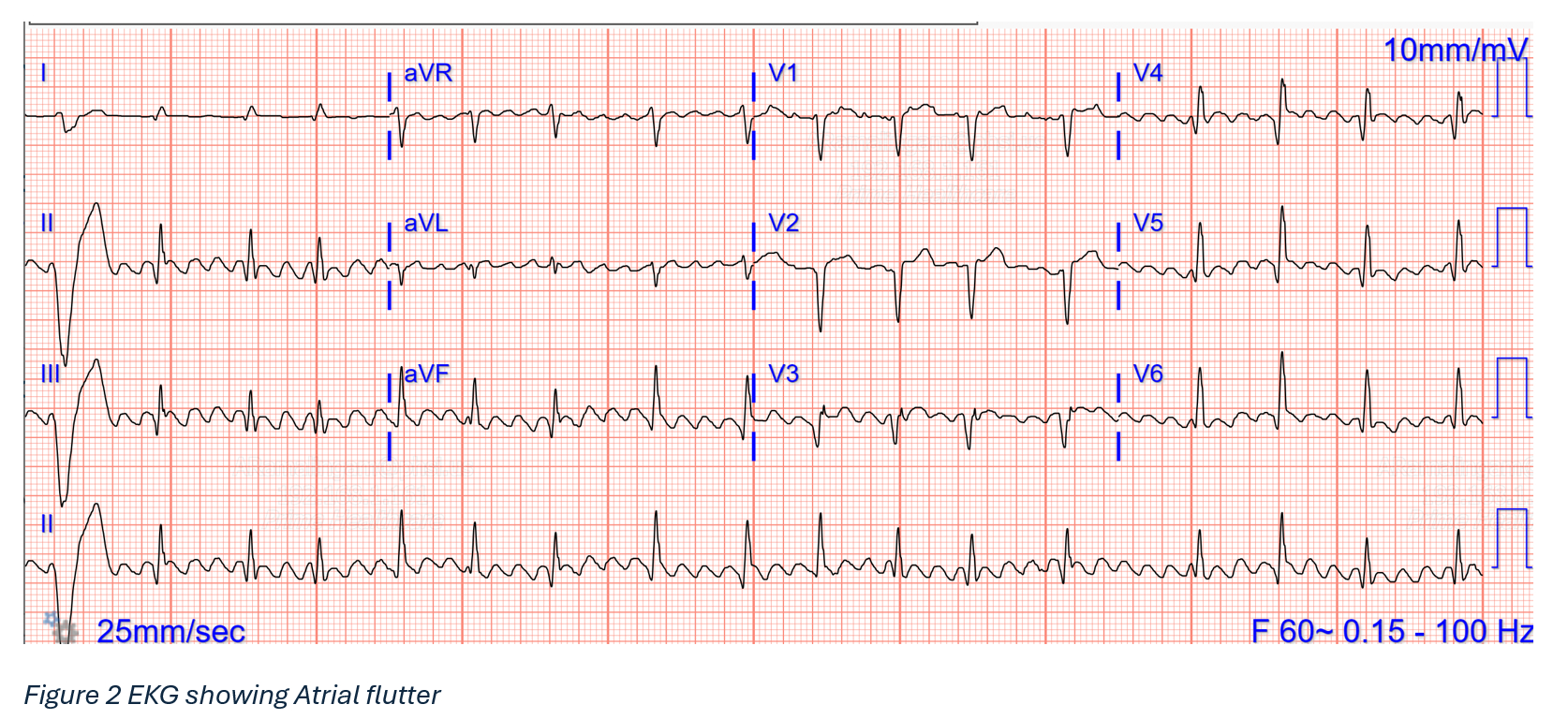
Description of the Case: A 62-year-old male was admitted with altered mental status, fever, hypotension, and respiratory distress. Initial workup revealed sepsis with severe hyponatremia (Na 114 mEq/L), acute kidney injury (Cr 1.54 mg/dL), elevated lactate (4.0 mmol/L), and rising troponin levels (195→483 ng/L). He developed transient atrial flutter that resolved spontaneously. Chest imaging showed right lower lobe infiltrates, and urine antigen testing confirmed Legionella pneumophila.
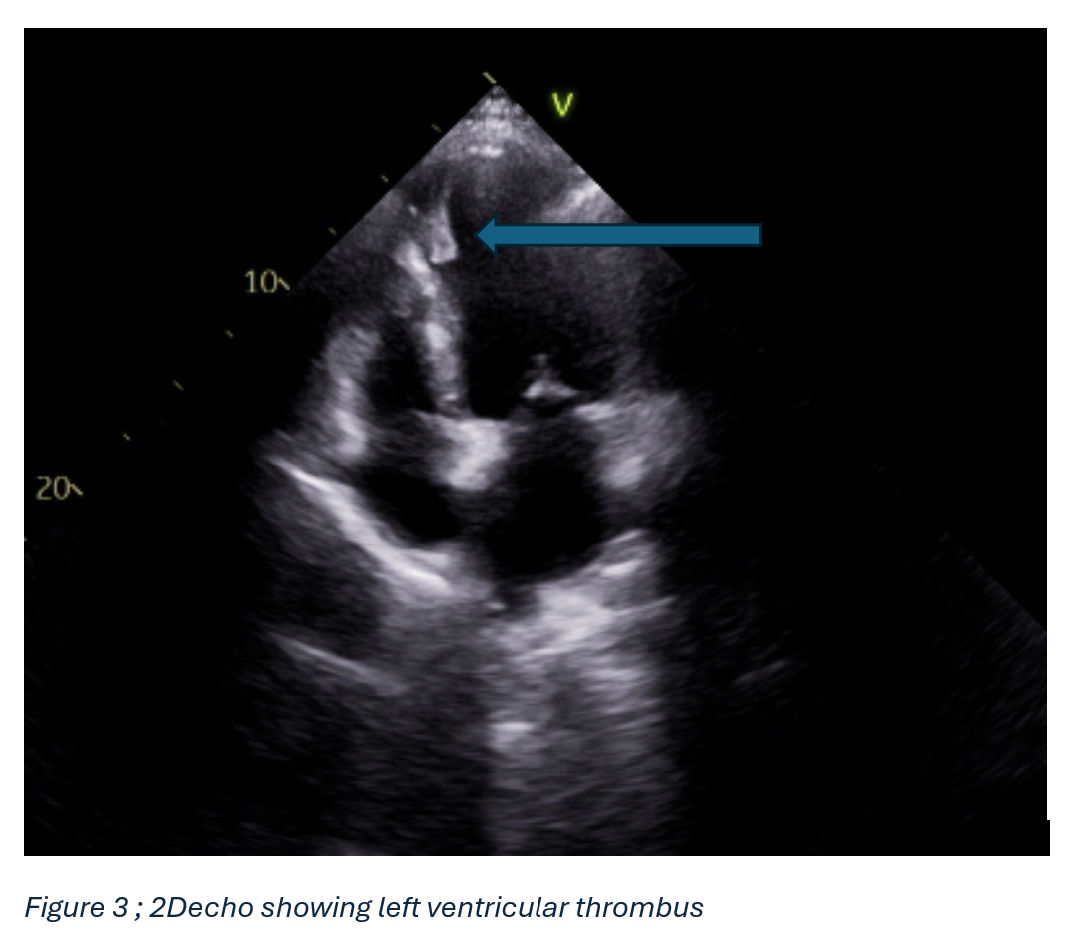
Echocardiography revealed severe global hypokinesis with an ejection fraction (EF) of 20–25% and an apical LV mural thrombus (2.8 × 1.2 cm). The cardiomyopathy was attributed to a combination of sepsis-related myocardial dysfunction and possible tachycardia-induced cardiomyopathy. He was managed with intravenous fluids, vasopressors, azithromycin, and anticoagulation (enoxaparin transitioning to apixaban).
Despite initial stabilization, the patient developed respiratory failure requiring intubation and intensive care support. With appropriate antimicrobial therapy and guideline-directed heart failure treatment (carvedilol, losartan), his cardiac function improved, and he was discharged to a rehabilitation facility on apixaban with close follow-up.
Discussion: Legionella pneumophila can lead to rare but serious cardiac complications, including myocarditis, endocarditis, and LV thrombus, due to bacterial invasion, inflammation, and sepsis-related dysfunction. In this case, reduced ejection fraction and severe hypokinesis resulted in a 2.8 × 1.2 cm LV thrombus, worsened by atrial flutter and tachycardia-induced cardiomyopathy. Effective management required coordinated anticoagulation and infection control. Legionnaires’ disease, often linked to contaminated water systems, is notifiable due to its outbreak risk. Early cardiac evaluation and prompt treatment are critical for improving outcomes in cases with cardiac involvement.
Description of the Case: A 62-year-old male was admitted with altered mental status, fever, hypotension, and respiratory distress. Initial workup revealed sepsis with severe hyponatremia (Na 114 mEq/L), acute kidney injury (Cr 1.54 mg/dL), elevated lactate (4.0 mmol/L), and rising troponin levels (195→483 ng/L). He developed transient atrial flutter that resolved spontaneously. Chest imaging showed right lower lobe infiltrates, and urine antigen testing confirmed Legionella pneumophila.
Echocardiography revealed severe global hypokinesis with an ejection fraction (EF) of 20–25% and an apical LV mural thrombus (2.8 × 1.2 cm). The cardiomyopathy was attributed to a combination of sepsis-related myocardial dysfunction and possible tachycardia-induced cardiomyopathy. He was managed with intravenous fluids, vasopressors, azithromycin, and anticoagulation (enoxaparin transitioning to apixaban).
Despite initial stabilization, the patient developed respiratory failure requiring intubation and intensive care support. With appropriate antimicrobial therapy and guideline-directed heart failure treatment (carvedilol, losartan), his cardiac function improved, and he was discharged to a rehabilitation facility on apixaban with close follow-up.
Discussion: Legionella pneumophila can lead to rare but serious cardiac complications, including myocarditis, endocarditis, and LV thrombus, due to bacterial invasion, inflammation, and sepsis-related dysfunction. In this case, reduced ejection fraction and severe hypokinesis resulted in a 2.8 × 1.2 cm LV thrombus, worsened by atrial flutter and tachycardia-induced cardiomyopathy. Effective management required coordinated anticoagulation and infection control. Legionnaires’ disease, often linked to contaminated water systems, is notifiable due to its outbreak risk. Early cardiac evaluation and prompt treatment are critical for improving outcomes in cases with cardiac involvement.
More abstracts on this topic:
Gastrointestinal Bleeding Risk: Diltiazem versus Metoprolol in Patients on Rivaroxaban, Apixaban, or Dabigatran.
Seylani Allen, Haile Yohannes, Asiedu Samuel, Shahin Hania
6-Nitrodopamine potentiates the positive chronotopic and inotropic effect induced by noradrenaline in the rat isolated heartLima Antonio, Sobanski Joao Fernando, Antunes Edson, De Nucci Gilberto