Final ID: MP1542
Diverging Trends in Cardiovascular Mortality: A Comparative Analysis of GBD and CDC WONDER for Five Conditions (1999–2020)
Abstract Body (Do not enter title and authors here): Background
Understanding cardiovascular mortality is key for shaping public health priorities. Two major sources in the U.S.—CDC WONDER and the Global Burden of Disease (GBD) study—report mortality differently. While CDC WONDER reflects death certificate data, GBD employs modeling techniques and redistributes ill-defined ("garbage") codes to improve cause of death attribution. Prior comparisons have focused on ischemic heart disease and stroke, but other cardiovascular conditions remain understudied.
Methods
We examined trends in valvular heart disease (I34.0-I37.9), hypertensive heart disease (I11.0, I11.9), peripheral arterial disease (I70.2), infective endocarditis (I38), and aortic aneurysm (I71) using both databases from 1999–2020. Annual U.S. mortality data from GBD and CDC WONDER were analyzed. For each condition, absolute deaths and crude mortality rates (CMRs) per 100,000 population were extracted. Percent change from 1999 to 2020 was calculated. CMRs were reported with 95% uncertainty intervals (UI) for GBD and 95% confidence intervals (CI) for CDC WONDER.
Results
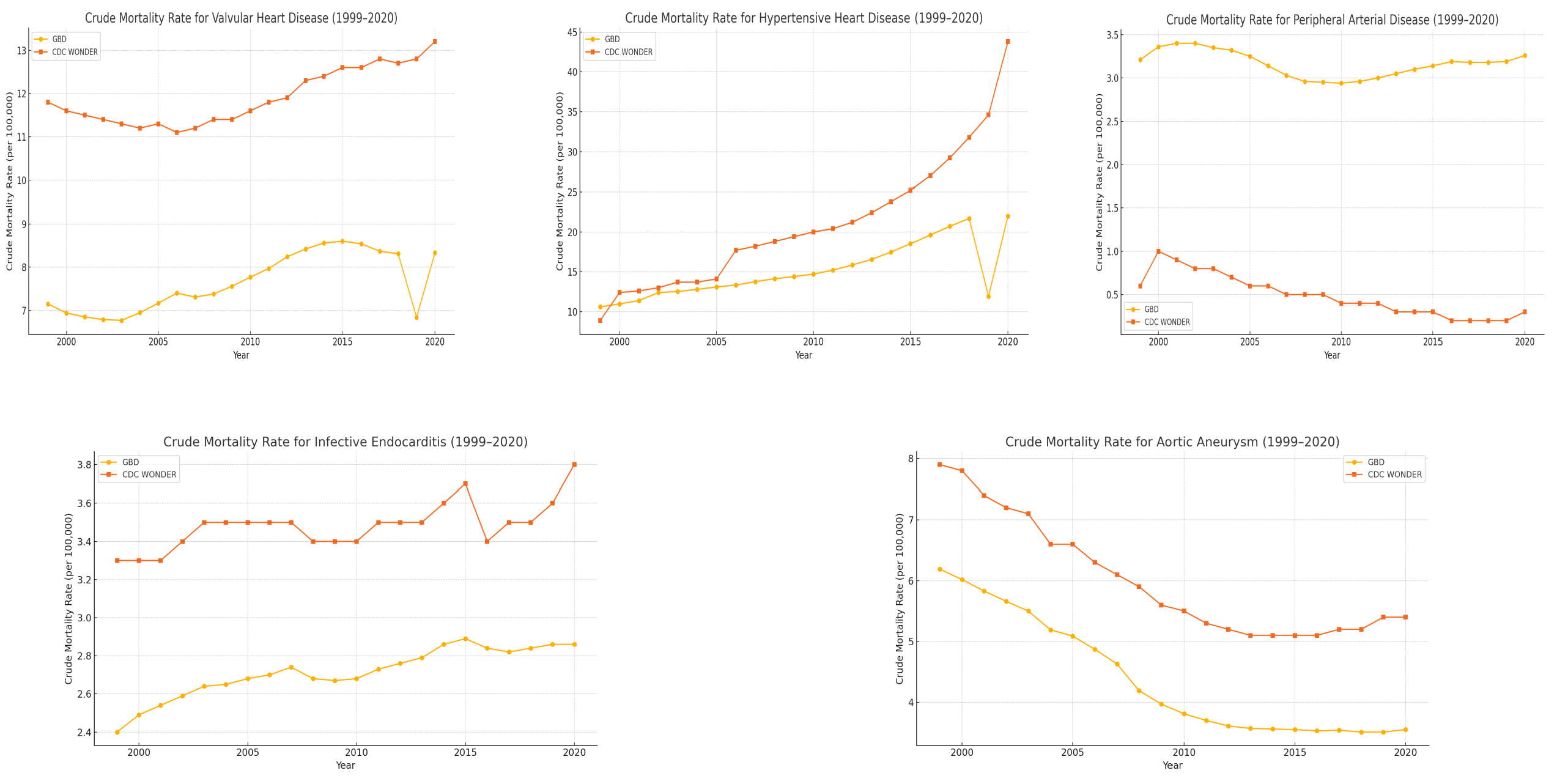
Substantial differences were found between the databases. Valvular heart disease deaths rose by 38.8% (GBD) and 32.2% (CDC). CMRs increased from 7.15 (UI: 7.62–6.18) to 8.33 (9.12–6.74) in GBD and from 11.8 (CI: 11.7–11.9) to 13.2 (13.1–13.4) in CDC. Hypertensive heart disease exhibited the most pronounced increase where deaths rose by 147.2% (GBD) and 474.7% (CDC). GBD CMRs rose from 10.6 (11.2–9.46) to 22.0 (23.62–19.21); CDC from 8.9 (9.2–8.9) to 43.8 (44.3–43.8). Peripheral arterial disease deaths rose 20.9% (GBD) but fell 50.4% (CDC). CMRs changed from 3.21 (3.45–2.82) to 3.26 (3.55–2.78) in GBD and from 0.6 (0.6–0.7) to 0.3 (0.3–0.3) in CDC. Infective endocarditis deaths increased by 41.9% (GBD) and 36.4% (CDC). CMRs rose from 2.4 (2.53–2.17) to 2.86 (3.07–2.50) in GBD and from 3.3 (3.4–3.3) to 3.8 (3.9–3.8) in CDC. Aortic aneurysm deaths declined 31.6% (GBD) and 18.9% (CDC). GBD CMRs fell from 6.19 (6.45–5.63) to 3.55 (3.76–3.15); CDC from 7.9 (8.0–7.8) to 5.4 (5.5–5.3).
Conclusion
Cardiovascular mortality trends varied significantly between GBD and CDC WONDER. Differences were especially striking in hypertensive heart disease and peripheral arterial disease, likely due to methodological variation in death coding and redistribution. Awareness of these discrepancies is crucial for interpreting national mortality data and informing policy.
Understanding cardiovascular mortality is key for shaping public health priorities. Two major sources in the U.S.—CDC WONDER and the Global Burden of Disease (GBD) study—report mortality differently. While CDC WONDER reflects death certificate data, GBD employs modeling techniques and redistributes ill-defined ("garbage") codes to improve cause of death attribution. Prior comparisons have focused on ischemic heart disease and stroke, but other cardiovascular conditions remain understudied.
Methods
We examined trends in valvular heart disease (I34.0-I37.9), hypertensive heart disease (I11.0, I11.9), peripheral arterial disease (I70.2), infective endocarditis (I38), and aortic aneurysm (I71) using both databases from 1999–2020. Annual U.S. mortality data from GBD and CDC WONDER were analyzed. For each condition, absolute deaths and crude mortality rates (CMRs) per 100,000 population were extracted. Percent change from 1999 to 2020 was calculated. CMRs were reported with 95% uncertainty intervals (UI) for GBD and 95% confidence intervals (CI) for CDC WONDER.
Results
Substantial differences were found between the databases. Valvular heart disease deaths rose by 38.8% (GBD) and 32.2% (CDC). CMRs increased from 7.15 (UI: 7.62–6.18) to 8.33 (9.12–6.74) in GBD and from 11.8 (CI: 11.7–11.9) to 13.2 (13.1–13.4) in CDC. Hypertensive heart disease exhibited the most pronounced increase where deaths rose by 147.2% (GBD) and 474.7% (CDC). GBD CMRs rose from 10.6 (11.2–9.46) to 22.0 (23.62–19.21); CDC from 8.9 (9.2–8.9) to 43.8 (44.3–43.8). Peripheral arterial disease deaths rose 20.9% (GBD) but fell 50.4% (CDC). CMRs changed from 3.21 (3.45–2.82) to 3.26 (3.55–2.78) in GBD and from 0.6 (0.6–0.7) to 0.3 (0.3–0.3) in CDC. Infective endocarditis deaths increased by 41.9% (GBD) and 36.4% (CDC). CMRs rose from 2.4 (2.53–2.17) to 2.86 (3.07–2.50) in GBD and from 3.3 (3.4–3.3) to 3.8 (3.9–3.8) in CDC. Aortic aneurysm deaths declined 31.6% (GBD) and 18.9% (CDC). GBD CMRs fell from 6.19 (6.45–5.63) to 3.55 (3.76–3.15); CDC from 7.9 (8.0–7.8) to 5.4 (5.5–5.3).
Conclusion
Cardiovascular mortality trends varied significantly between GBD and CDC WONDER. Differences were especially striking in hypertensive heart disease and peripheral arterial disease, likely due to methodological variation in death coding and redistribution. Awareness of these discrepancies is crucial for interpreting national mortality data and informing policy.
More abstracts on this topic:
A Rare Case of Mycotic Pseudoaneurysm in a Pediatric Patient with a History of Disseminated MRSA
Amilhamja Anissa, Shaikh Adam, Porisch Mary
84 Immune checkpoint profiling in major aortic diseases leads to identification of potential roles of CD155-CD206 pathway in suppressing inflammation and immune responsesShao Ying, Saaoud Fatma, Xu Keman, Lu Yifan, Jiang Xiaohua, Wang Hong, Yang Xiaofeng