Final ID: Mo2092
Relationship of smoking to inflammation, coronary artery disease severity, and cardiovascular outcomes in patients with stable chest pain: Insights from the PROMISE randomized trial
Abstract Body (Do not enter title and authors here): Background: Smoking is related to systemic inflammation and is a major modifiable risk factor for coronary artery disease (CAD) and adverse cardiovascular (CV) outcomes. However, these associations have not been studied in low-to-intermediate risk symptomatic patients with suspected CAD.
Aim: To examine the role of smoking in promoting inflammation, and to assess its possible contribution to unfavorable CV test outcomes and adverse events in outpatients with stable chest pain.
Methods: Patients from the Prospective Multicenter Imaging Study for Evaluation of Chest Pain (PROMISE) with known smoking status and analyzable diagnostic testing were included. Noninvasive testing (coronary CT angiography or functional stress test) was used to evaluate for presence of a coronary stenosis ≥70% or inducible ischemia, respectively. Inflammatory biomarkers hsCRP, IL-6, and MMP-9 were compared between ever-smokers and nonsmokers. Multivariable logistic and Cox regressions were used to evaluate the associations of smoking with positive noninvasive (NI) testing and adverse events, adjusting for demographics and traditional CV risk factors. The primary end point was death, myocardial infarction, or unstable angina hospitalizations over a median follow-up of 24.4 months.
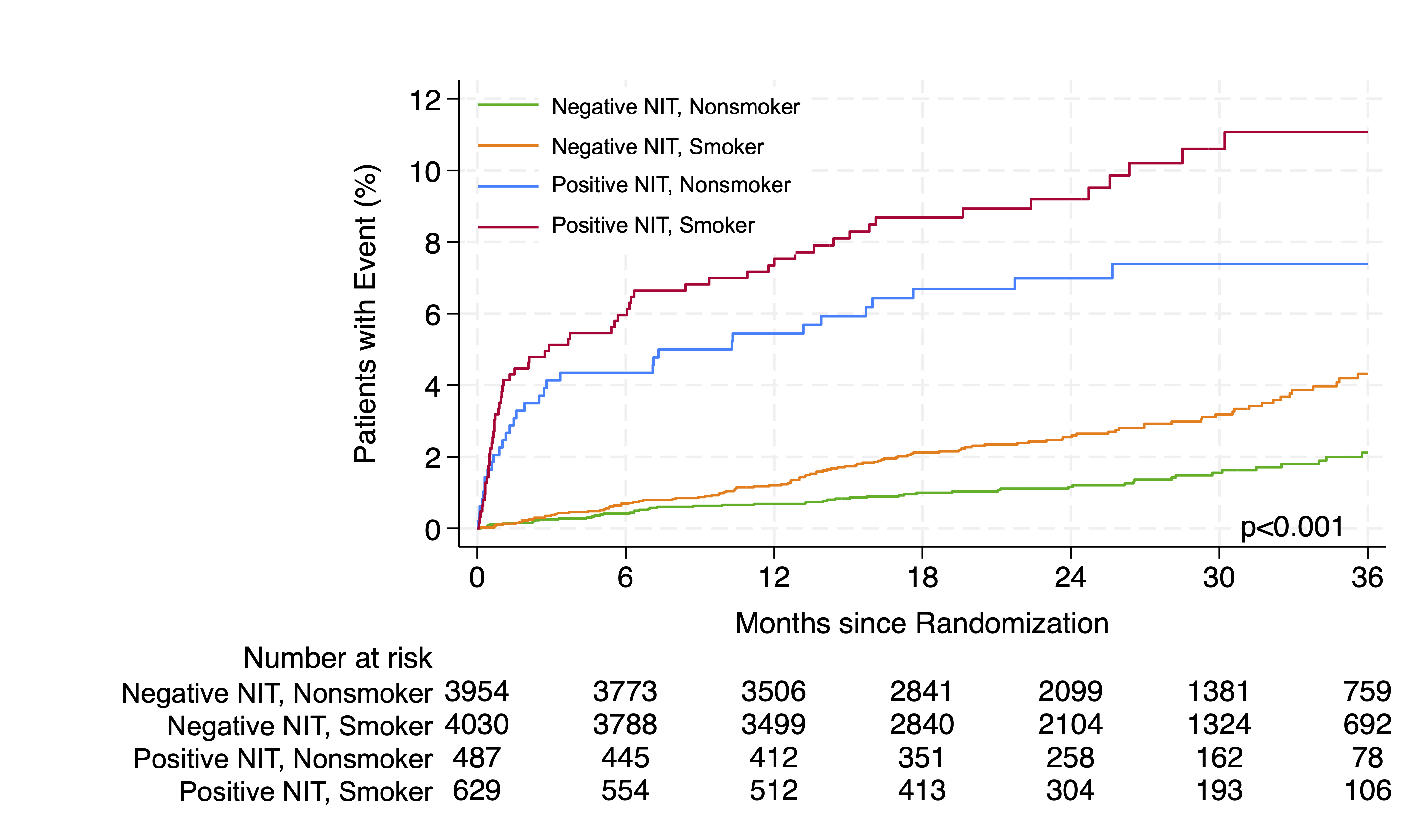
Results: A total of 9,100 patients (mean age 61±8 years; 52.6% female, 51.2% ever-smokers) were analyzed. Compared to non-smokers, smokers were slightly younger (60±8 vs 61±8 years, p<0.001), more often male (53% vs 42%, p<0.001), with higher median ASCVD risk (14% [IQR: 9-23] vs 8% [IQR: 4-15], p<0.001) and higher event rates (3.8% vs. 2.0%, p<0.001). Inflammatory biomarkers were higher among smokers (hsCRP +9%, p=0.008, IL-6 +12%, p<0.001, MMP-9 +22%, p<0.001). Smoking was independently related to positive NI test results (aOR 1.24, 95% CI 1.09-1.42) and events (aHR 1.75, 95% CI 1.35-2.26). Smoking was a strong event predictor in patients without significant test abnormality (aHR 2.05, 95% CI 1.49-2.84), but not in those with positive test results (aHR 1.32, 95% CI 0.87-2.02).
Conclusions: Among patients with stable chest pain, smoking was linked to greater inflammation, more frequent abnormal NI test results, and higher CV risk. This was particularly true in those with negative noninvasive testing, highlighting the need for early smoking cessation, even in patients with negative NI testing.
Aim: To examine the role of smoking in promoting inflammation, and to assess its possible contribution to unfavorable CV test outcomes and adverse events in outpatients with stable chest pain.
Methods: Patients from the Prospective Multicenter Imaging Study for Evaluation of Chest Pain (PROMISE) with known smoking status and analyzable diagnostic testing were included. Noninvasive testing (coronary CT angiography or functional stress test) was used to evaluate for presence of a coronary stenosis ≥70% or inducible ischemia, respectively. Inflammatory biomarkers hsCRP, IL-6, and MMP-9 were compared between ever-smokers and nonsmokers. Multivariable logistic and Cox regressions were used to evaluate the associations of smoking with positive noninvasive (NI) testing and adverse events, adjusting for demographics and traditional CV risk factors. The primary end point was death, myocardial infarction, or unstable angina hospitalizations over a median follow-up of 24.4 months.
Results: A total of 9,100 patients (mean age 61±8 years; 52.6% female, 51.2% ever-smokers) were analyzed. Compared to non-smokers, smokers were slightly younger (60±8 vs 61±8 years, p<0.001), more often male (53% vs 42%, p<0.001), with higher median ASCVD risk (14% [IQR: 9-23] vs 8% [IQR: 4-15], p<0.001) and higher event rates (3.8% vs. 2.0%, p<0.001). Inflammatory biomarkers were higher among smokers (hsCRP +9%, p=0.008, IL-6 +12%, p<0.001, MMP-9 +22%, p<0.001). Smoking was independently related to positive NI test results (aOR 1.24, 95% CI 1.09-1.42) and events (aHR 1.75, 95% CI 1.35-2.26). Smoking was a strong event predictor in patients without significant test abnormality (aHR 2.05, 95% CI 1.49-2.84), but not in those with positive test results (aHR 1.32, 95% CI 0.87-2.02).
Conclusions: Among patients with stable chest pain, smoking was linked to greater inflammation, more frequent abnormal NI test results, and higher CV risk. This was particularly true in those with negative noninvasive testing, highlighting the need for early smoking cessation, even in patients with negative NI testing.
More abstracts on this topic:
Assessing Trends in Disability-Adjusted Life Years (DALYs) and Age-Adjusted Mortality Rates (AAMR) of Ischemic Heart Disease: A Comparative Analysis of the United States and Global Burden of Disease
Buhadur Ali Muhammad Khan, Shahzaib Muhammad, Qureshi Muhammad Ahmad, Ammar Ur Rahman Mohammad, Munir Luqman, Khalid Amna, Hayat Malik Saad, Shoaib Muhammad Mukarram
Aortic Arch Calcification Improves Cardiovascular Event Risk Stratification Among Individuals With a History of Cigarette Smoke ExposureTrujillo Robert, Ansari Salman, Budoff Matthew, Mcclelland Robyn, Hansen Spencer, Szklo Moyses