Final ID: MP995
Prognostic Accuracy of the Systemic Immune-Inflammation Index for Atrial Fibrillation Recurrence Following Catheter Ablation: A Systematic Review and Meta-Analysis
Abstract Body (Do not enter title and authors here): Background: Atrial fibrillation (AF) recurrence remains a common and clinically significant complication following CA. Identifying reliable biomarkers for stratifying recurrence risk is essential to guide post-ablation management and improve long-term outcomes. The systemic immune-inflammation index (SII), a composite marker derived from peripheral platelets, neutrophils, and lymphocytes, has emerged as a potential predictor of cardiovascular events.
Methods: Embase, Medline (via PubMed), Scopus, and Web of Science were systematically searched from inception to May 2025 to identify studies evaluating the accuracy of the SII in predicting AF recurrence after CA. Pooled mean difference (MD) and area under the curve (AUC), along with 95% confidence intervals (CIs), were calculated using the inverse variance method under a random-effects model. Pooled sensitivity and specificity, with corresponding 95% CIs, were estimated using a bivariate random-effects model with Meta-DiSc V2.
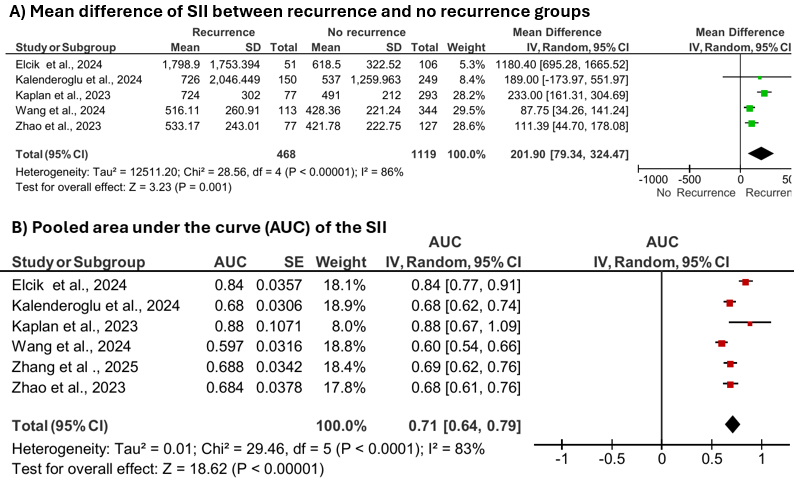
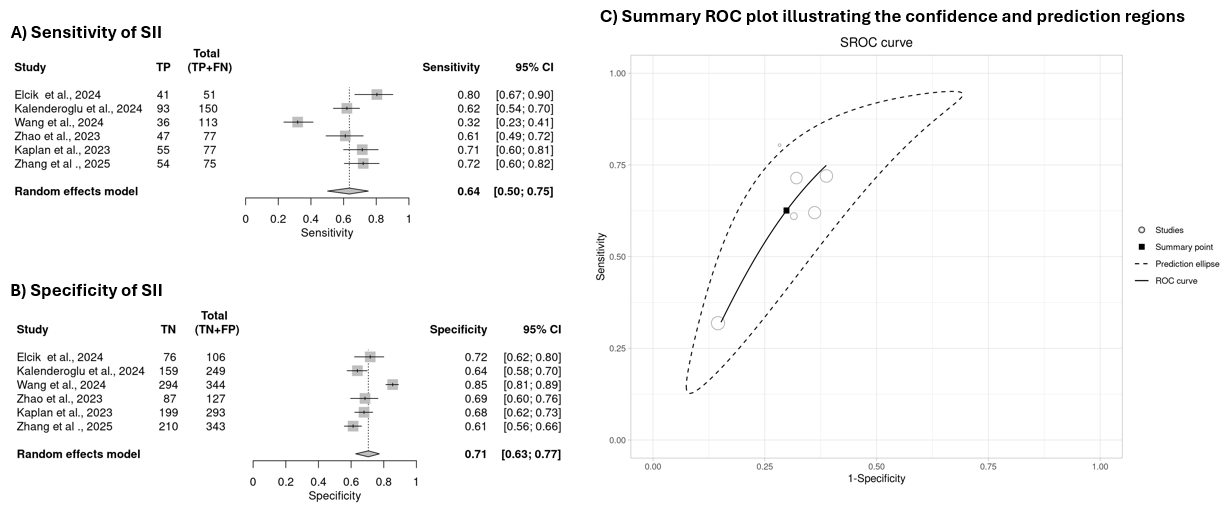
Results: Six studies comprising 543 patients with recurrence and 1,462 without recurrence were included. AF recurrence was significantly associated with higher SII levels (MD: 201.9; 95% CI: 79.34, 324.47; p=0.001). The pooled AUC for SII was 0.71 (95% CI: 0.64, 0.79; p<0.00001), indicating moderate discriminative ability. Diagnostic accuracy analysis confirmed SII as a reliable predictor of recurrence, with a pooled sensitivity of 64% (95% CI: 0.50, 0.75), specificity of 71% (95% CI: 0.63, 0.77), positive likelihood ratio (PLR) of 2.09 (95% CI: 1.82, 2.40), and negative likelihood ratio (NLR) of 0.53 (95% CI: 0.41, 0.68). The 95% prediction ellipse area was 0.155.
Conclusion: The SII demonstrates potential as a biomarker for identifying patients at elevated risk of AF recurrence following CA. In line with current trends emphasizing inflammation’s role in arrhythmogenesis, these findings support incorporating immune-inflammatory profiling into post-ablation risk assessment. Although not yet incorporated into existing clinical guidelines, the evidence underscores the need for its consideration in future guideline updates as part of a multi-parametric approach that integrates clinical, electrophysiological, imaging, and biomarker-based data to guide post-ablation management and improve patient outcomes.
Methods: Embase, Medline (via PubMed), Scopus, and Web of Science were systematically searched from inception to May 2025 to identify studies evaluating the accuracy of the SII in predicting AF recurrence after CA. Pooled mean difference (MD) and area under the curve (AUC), along with 95% confidence intervals (CIs), were calculated using the inverse variance method under a random-effects model. Pooled sensitivity and specificity, with corresponding 95% CIs, were estimated using a bivariate random-effects model with Meta-DiSc V2.
Results: Six studies comprising 543 patients with recurrence and 1,462 without recurrence were included. AF recurrence was significantly associated with higher SII levels (MD: 201.9; 95% CI: 79.34, 324.47; p=0.001). The pooled AUC for SII was 0.71 (95% CI: 0.64, 0.79; p<0.00001), indicating moderate discriminative ability. Diagnostic accuracy analysis confirmed SII as a reliable predictor of recurrence, with a pooled sensitivity of 64% (95% CI: 0.50, 0.75), specificity of 71% (95% CI: 0.63, 0.77), positive likelihood ratio (PLR) of 2.09 (95% CI: 1.82, 2.40), and negative likelihood ratio (NLR) of 0.53 (95% CI: 0.41, 0.68). The 95% prediction ellipse area was 0.155.
Conclusion: The SII demonstrates potential as a biomarker for identifying patients at elevated risk of AF recurrence following CA. In line with current trends emphasizing inflammation’s role in arrhythmogenesis, these findings support incorporating immune-inflammatory profiling into post-ablation risk assessment. Although not yet incorporated into existing clinical guidelines, the evidence underscores the need for its consideration in future guideline updates as part of a multi-parametric approach that integrates clinical, electrophysiological, imaging, and biomarker-based data to guide post-ablation management and improve patient outcomes.
More abstracts on this topic:
Changes in decisional conflict among adults with atrial fibrillation viewing a rhythm management decision aid: Results from a single-arm feasibility trial
Reading Turchioe Meghan, Shamnath Afra, Zhao Yihong, Volodarskiy Alexander, Slotwiner David, Biviano Angelo
Ablation for Atrial Fibrillation: A Comprehensive Meta-Analysis of Randomized Controlled Trials with Reconstructed Time-to-Event DataMi Jiaqi, Katapadi Aashish, Darden Douglas, Uppalapati Sree Varuntej, Kabra Aanya, Katapadi Aashika